Overview
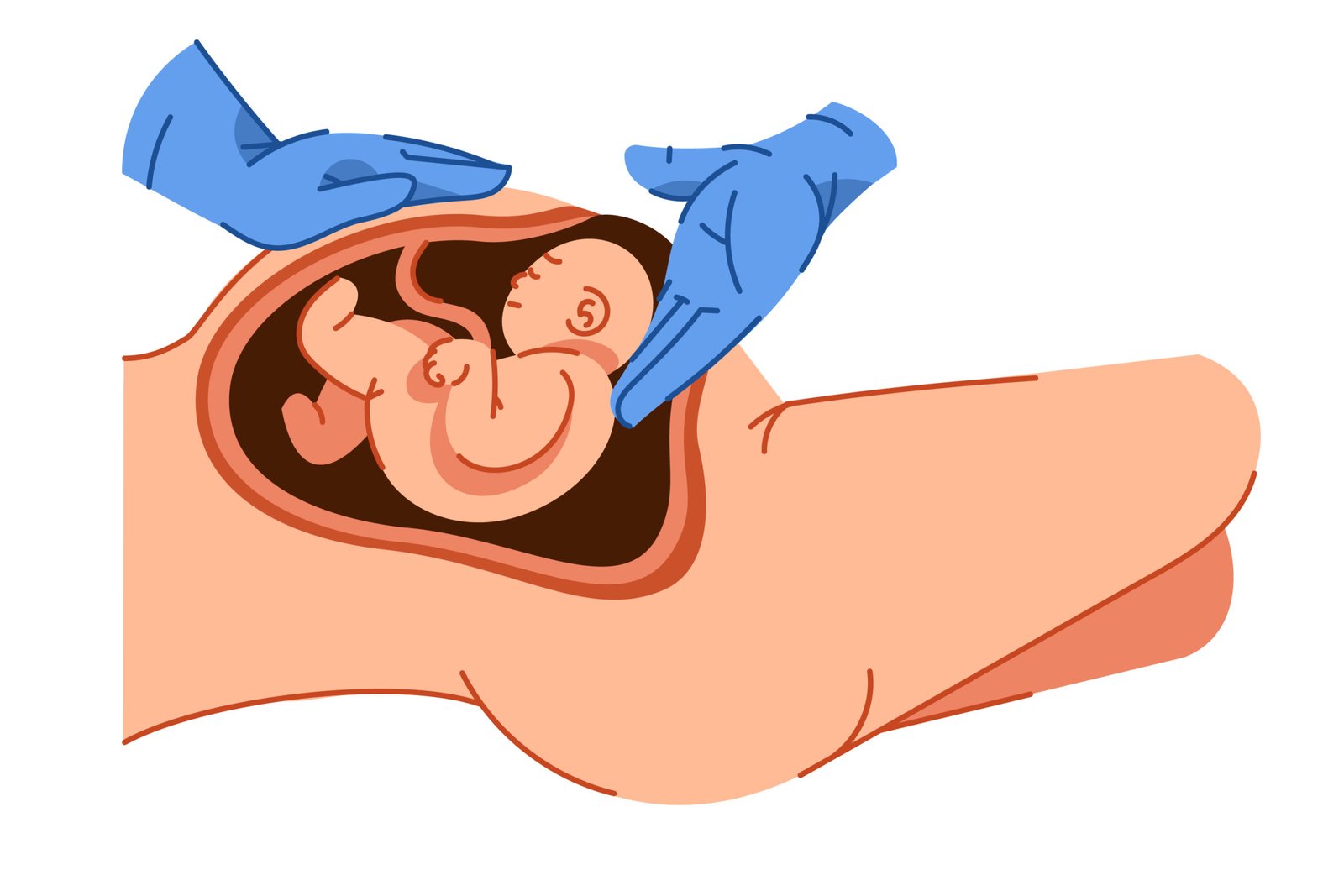
Umbilical Cord Prolapse is an obstetric emergency that occurs when the umbilical cord slips through the cervix and into the birth canal ahead of the baby during labor. This condition can compromise blood flow and oxygen delivery to the fetus, posing a serious risk of injury or death if not treated immediately. Prompt medical intervention, often by emergency cesarean delivery, is crucial to ensure a positive outcome for both the baby and the mother.
What is Umbilical Cord Prolapse
Umbilical Cord Prolapse is a childbirth complication in which the umbilical cord descends through the cervix before or alongside the presenting part of the fetus, usually the head. As labor progresses, the cord can become compressed between the baby and the walls of the birth canal, reducing or cutting off oxygen and nutrient flow to the fetus. It is a rare condition, occurring in about 1 in 300 live births, but one that requires immediate recognition and intervention to prevent fetal distress or death.
Symptoms
- Sudden, visible cord protruding from the vagina during labor
- Fetal heart rate abnormalities (bradycardia or decelerations) detected on fetal monitoring
- Sudden onset of excessive fetal movement followed by reduced movement
- Vaginal bleeding (in some cases)
- No maternal symptoms in many cases—diagnosed during a pelvic exam or through fetal monitoring
Causes
Umbilical Cord Prolapse typically results from a disruption in the normal positioning of the baby and the cord. Common causes include:
- Premature rupture of membranes, especially when the baby’s head has not engaged
- Abnormal fetal presentation, such as breech or transverse lie
- Multiple pregnancies (twins, triplets)
- Polyhydramnios (excessive amniotic fluid)
- Long umbilical cord
- Artificial rupture of membranes before fetal head engagement
- High station of fetal head during labor
Risk Factors
- Prematurity (before 37 weeks gestation)
- Low birth weight infants
- Excessive amniotic fluid (polyhydramnios)
- Breech or transverse fetal position
- Multiple gestation
- Use of amniotomy (artificial rupture of membranes)
- High parity (multiple previous births)
- Placenta previa or marginal cord insertion
Complications
- Fetal hypoxia (lack of oxygen) due to cord compression
- Brain injury or cerebral palsy in severe or prolonged cases
- Stillbirth, if not treated promptly
- Emergency cesarean section and associated maternal risks
- Increased neonatal intensive care unit (NICU) admissions
- Maternal psychological distress from traumatic birth experience
Prevention
While not all cases can be prevented, several strategies can reduce the risk of umbilical cord prolapse:
- Avoiding artificial rupture of membranes when the baby’s head is not engaged
- Careful monitoring during labor, especially with known risk factors
- Ultrasound assessment of fetal position and amniotic fluid volume
- Hospital delivery for high-risk pregnancies to ensure rapid intervention
- Close prenatal supervision in cases with breech presentation or multiple gestation
- Elective cesarean delivery in cases with high risk of prolapse
Treatment Options in Korea
Korea offers advanced, well-coordinated obstetric care capable of managing obstetric emergencies like umbilical cord prolapse effectively:
- Immediate recognition using fetal heart rate monitoring and physical examination
- Manual elevation of the presenting part to reduce pressure on the cord while preparing for delivery
- Maternal positioning (e.g., Trendelenburg or knee-chest) to relieve cord compression
- Oxygen administration to the mother to optimize fetal oxygenation
- Emergency cesarean section: The definitive treatment in most cases
- Neonatal resuscitation and intensive care, if needed after delivery
- Post-delivery monitoring and emotional support for the mother
With rapid intervention and access to high-level maternity and neonatal care, South Korea achieves excellent outcomes in managing umbilical cord prolapse cases.