Overview
Tularaemia, also known as rabbit fever or deer fly fever, is a rare infectious disease caused by the bacterium Francisella tularensis. It primarily affects wild animals such as rabbits, rodents, and ticks, but can also infect humans through direct contact, insect bites, inhalation, or contaminated food and water. While uncommon in South Korea, tularaemia is considered a zoonotic disease, and Korean healthcare authorities maintain awareness for early detection, particularly among hunters, farmers, and laboratory personnel. Modern diagnostic techniques, antibiotics, and preventive measures ensure effective management and minimize complications.
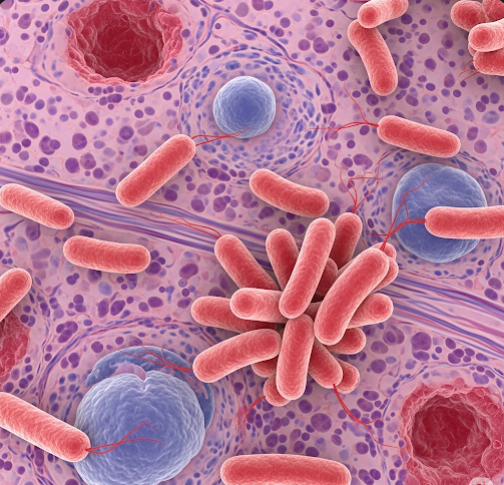
What is Tularaemia?
Tularaemia is a bacterial infection that can present in several clinical forms depending on the route of entry of Francisella tularensis. The disease is highly infectious, and only a small number of bacteria are required to cause infection. Tularaemia is classified into different types:
- Ulceroglandular: Characterized by skin ulcers and swollen lymph nodes, usually following a tick or insect bite
- Glandular: Swelling of lymph nodes without visible skin ulcers
- Oculoglandular: Eye infection caused by direct contact with contaminated material
- Oropharyngeal: Infection through ingestion of contaminated food or water, leading to sore throat and gastrointestinal symptoms
- Pneumonic: Lung infection caused by inhalation of bacteria, potentially severe
- Typhoidal: Systemic infection with fever and malaise without localized lesions
South Korean healthcare facilities employ modern laboratory techniques such as polymerase chain reaction (PCR), serology, and culture to accurately diagnose tularaemia.
Symptoms
Symptoms of tularaemia vary depending on the form of infection but often include:
- Fever, chills, and fatigue
- Headache and body aches
- Ulcers at the site of infection (in ulceroglandular form)
- Swollen and tender lymph nodes
- Sore throat, mouth ulcers, and gastrointestinal upset in oropharyngeal tularaemia
- Respiratory symptoms such as cough, chest pain, and difficulty breathing in pneumonic tularaemia
- Conjunctivitis or eye irritation in oculoglandular cases
- Nausea, vomiting, and abdominal pain in typhoidal tularaemia
Symptoms usually appear 3 to 5 days after exposure, but incubation can range from 1 to 14 days. Early recognition in Korean medical centers is key to prompt treatment.
Causes
Tularaemia is caused by infection with Francisella tularensis, a highly virulent bacterium. The bacteria can enter the human body through several routes:
- Insect bites: Ticks, deer flies, and mosquitoes carrying the bacteria
- Direct contact: Handling infected animals, such as rabbits, rodents, or wildlife carcasses
- Inhalation: Breathing in contaminated dust or aerosols
- Ingestion: Consuming contaminated water or undercooked meat
- Laboratory exposure: Handling bacteria in research or diagnostic labs
Understanding these routes allows Korean health authorities to advise preventive measures for high-risk populations.
Risk Factors
Certain factors increase the risk of tularaemia:
- Occupational exposure: Hunters, farmers, veterinarians, and laboratory workers
- Outdoor activities in rural or wooded areas with wild animal populations
- Handling or skinning wild animals without protective equipment
- Drinking untreated water from natural sources
- Weakened immune system due to chronic illness or immunosuppressive therapy
Risk awareness campaigns and protective guidelines in South Korea help reduce exposure among vulnerable groups.
Complications
If untreated, tularaemia can lead to serious complications:
- Severe pneumonic tularaemia: Can cause respiratory failure and require intensive care
- Systemic infection: Typhoidal tularaemia may lead to sepsis and organ failure
- Chronic infection: Lymph node abscesses or persistent fatigue
- Secondary infections: Particularly in immunocompromised individuals
- Eye damage: Untreated oculoglandular tularaemia can lead to vision problems
- Gastrointestinal complications: Ulcers, dehydration, and malnutrition in oropharyngeal cases
Timely antibiotic treatment in South Korea effectively reduces these risks and improves recovery.
Prevention
Prevention of tularaemia focuses on minimizing exposure to the bacteria:
- Avoid direct contact with wild animals, particularly sick or dead ones
- Use gloves and protective clothing when handling animals or cleaning animal habitats
- Employ insect repellents and protective clothing to prevent tick and insect bites
- Drink only treated or boiled water in outdoor or rural areas
- Practice proper food hygiene, including thorough cooking of meat
- Laboratory personnel should follow strict biosafety protocols
Public health education and preventive measures in Korea ensure that high-risk populations are informed and protected.
Treatment Options in Korea
Tularaemia is treatable with prompt antibiotic therapy, and South Korea offers modern medical care for effective management:
Diagnosis:
- Blood tests and serology to detect antibodies
- PCR testing for bacterial DNA
- Culture of samples from ulcers, lymph nodes, or respiratory secretions
- Imaging studies if internal organs are affected
Medical Treatments:
- Antibiotics: Streptomycin, gentamicin, doxycycline, or ciprofloxacin depending on severity
- Supportive care: Hydration, fever management, and pain relief
- Hospitalization: For severe pneumonic or systemic cases requiring intensive monitoring
Follow-up and Monitoring:
- Regular monitoring to ensure bacterial clearance
- Assessment for long-term complications such as persistent lymph node swelling or lung damage
- Patient education on avoiding future exposures
South Korea combines advanced diagnostic tools, effective antibiotic regimens, and public health measures to manage tularaemia, ensuring rapid recovery and minimizing the risk of outbreaks.