Overview
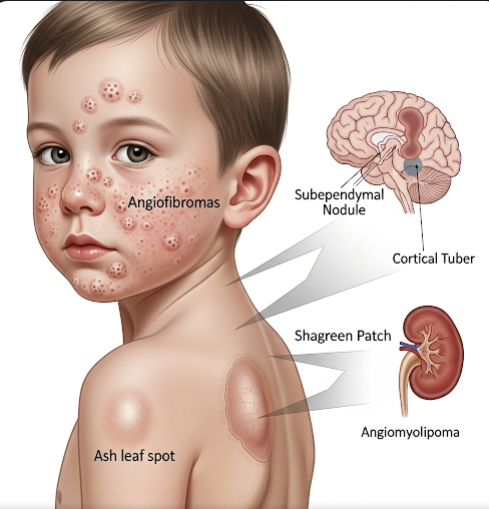
Tuberous Sclerosis Complex (TSC) is a rare genetic disorder characterized by the growth of benign tumors in multiple organs, including the brain, skin, kidneys, heart, and lungs. These growths can lead to a wide range of neurological, dermatological, and systemic symptoms. In South Korea, advanced genetic testing, imaging techniques, and multidisciplinary management are available to diagnose and treat TSC. Early intervention is crucial to reduce complications, improve quality of life, and provide support for patients and families. TSC affects individuals differently, making personalized care essential.
What is Tuberous Sclerosis Complex?
Tuberous Sclerosis Complex is caused by mutations in either the TSC1 or TSC2 genes, which are responsible for regulating cell growth and division. The mutations lead to uncontrolled cell proliferation, forming hamartomas—benign tumor-like growths—across multiple organ systems. TSC is an autosomal dominant disorder, meaning a single copy of the mutated gene can cause the disease. Symptoms vary widely, with some individuals experiencing mild skin manifestations while others face severe neurological or organ complications. Korean healthcare centers utilize genetic testing, MRI, CT scans, and echocardiography to assess the extent of organ involvement.
Symptoms
Symptoms of TSC differ based on the organs affected and the severity of tumor growth:
Neurological Symptoms:
- Seizures, often beginning in infancy (infantile spasms)
- Developmental delays or intellectual disabilities
- Behavioral problems including autism spectrum disorder, ADHD, or anxiety
- Headaches and coordination difficulties
Dermatological Symptoms:
- Hypomelanotic macules (white patches on the skin)
- Facial angiofibromas (reddish bumps on the face)
- Shagreen patches (thickened skin areas, often on the back)
- Ungual or periungual fibromas (growths around nails)
Renal Symptoms:
- Angiomyolipomas (benign kidney tumors)
- Cysts or abnormal kidney growth
- Risk of kidney failure in severe cases
Cardiac Symptoms:
- Rhabdomyomas (benign heart tumors), particularly in infants
- Arrhythmias or obstruction of blood flow in severe cases
Pulmonary Symptoms:
- Lymphangioleiomyomatosis (LAM) in adult women, causing breathing difficulties
Symptoms can appear in infancy or develop later in childhood and adulthood, requiring continuous monitoring in Korea.
Causes
TSC is caused by mutations in the TSC1 gene (encoding hamartin) or the TSC2 gene (encoding tuberin). These proteins normally regulate the mTOR signaling pathway, which controls cell growth and proliferation. Mutations lead to unregulated cell division and tumor formation. Causes include:
- Inherited mutations: Autosomal dominant inheritance from an affected parent
- De novo mutations: New genetic mutations that occur spontaneously, accounting for most cases
Environmental or lifestyle factors do not cause TSC, although early diagnosis and monitoring can prevent complications.
Risk Factors
Key risk factors for TSC include:
- Family history of Tuberous Sclerosis Complex
- Known genetic mutations in TSC1 or TSC2 genes
- Sporadic occurrence, which can affect anyone with no prior family history
Genetic counseling is strongly recommended in South Korea for families with affected members to assess risks and guide family planning.
Complications
TSC can lead to multiple complications depending on the organs involved:
- Neurological: Uncontrolled seizures, intellectual disability, developmental delays
- Renal: Angiomyolipomas may rupture, causing bleeding or kidney failure
- Cardiac: Heart tumors can obstruct blood flow or cause arrhythmias
- Pulmonary: LAM may lead to progressive respiratory failure in women
- Skin: Cosmetic concerns from facial lesions affecting psychosocial well-being
- Overall health: Increased risk of complications from multi-organ involvement, requiring lifelong monitoring
In South Korea, multidisciplinary care teams work to manage these complications proactively and minimize long-term risks.
Prevention
While TSC cannot be prevented due to its genetic nature, early detection and monitoring can reduce the impact of complications:
- Prenatal genetic testing: For at-risk families to detect mutations early
- Regular imaging: MRI, CT scans, and echocardiography to monitor organ involvement
- Seizure management: Early treatment of neurological symptoms
- Behavioral and educational support: For developmental or psychiatric challenges
- Patient education: Encouraging routine health checks and symptom awareness
Korean medical centers emphasize early intervention and family education to ensure optimal outcomes for TSC patients.
Treatment Options in Korea
Treatment for TSC is individualized and focuses on symptom management, complication prevention, and improving quality of life:
Diagnosis:
- Genetic testing for TSC1 or TSC2 mutations
- MRI or CT scans for brain, kidney, and other organ assessment
- Echocardiography for cardiac tumor evaluation
- Pulmonary function tests for LAM monitoring
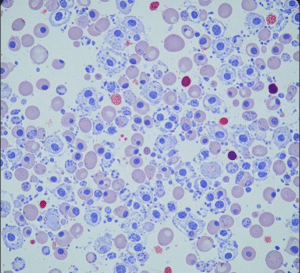
Medical Treatments:
- Antiepileptic drugs: To control seizures, including infantile spasms
- mTOR inhibitors (everolimus, sirolimus): Reduce tumor growth in kidneys, brain, and skin
- Pain management: For complications related to tumors or organ involvement
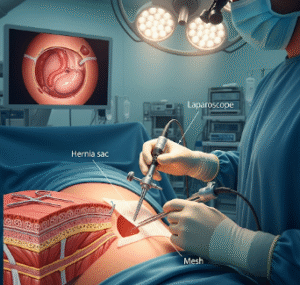
Surgical and Procedural Treatments:
- Surgical removal or embolization of renal or cardiac tumors if causing symptoms
- Laser therapy for facial angiofibromas
- Epilepsy surgery in refractory seizure cases
Supportive Care:
- Developmental and behavioral therapy for cognitive or psychiatric issues
- Educational support tailored to the child’s learning needs
- Regular follow-up with neurologists, nephrologists, cardiologists, dermatologists, and pulmonologists
- Family counseling and patient support groups
In Korea, multidisciplinary clinics provide comprehensive care, combining cutting-edge medical therapies with psychosocial support to optimize outcomes for TSC patients.