Overview
Tuberculosis (TB) is a contagious bacterial infection caused by Mycobacterium tuberculosis, primarily affecting the lungs but capable of impacting other organs such as the kidneys, spine, and brain. TB remains a major global health concern, including in South Korea, where public health authorities have implemented extensive screening, vaccination, and treatment programs. TB can be latent, causing no symptoms, or active, leading to persistent cough, fever, weight loss, and severe health complications if untreated. South Korea provides comprehensive TB management through advanced diagnostics, effective antibiotic regimens, and public health interventions to control transmission and improve patient outcomes.
What is Tuberculosis?
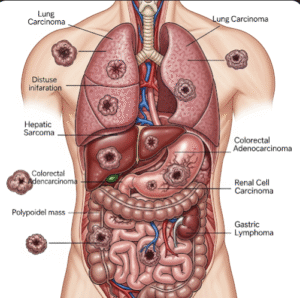
Tuberculosis is an infectious disease transmitted via airborne droplets when an infected person coughs, sneezes, or talks. While the lungs are the primary site of infection (pulmonary TB), the bacteria can spread to other parts of the body (extrapulmonary TB), including lymph nodes, bones, kidneys, and the central nervous system. TB exists in two forms:
- Latent TB infection (LTBI): The bacteria remain dormant, causing no symptoms, but can reactivate later
- Active TB disease: The bacteria multiply and cause clinical symptoms, making the individual contagious
In South Korea, TB diagnosis and management are supported by specialized clinics, national TB control programs, and advanced laboratory testing.
Symptoms
Symptoms of active TB vary depending on the site of infection but typically include:
- Persistent cough lasting more than two weeks, sometimes producing blood-streaked sputum
- Fever, often low-grade and occurring in the evening
- Night sweats
- Unexplained weight loss and loss of appetite
- Fatigue and general weakness
- Chest pain or shortness of breath in pulmonary TB
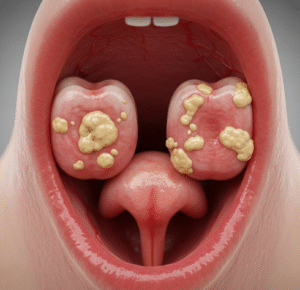
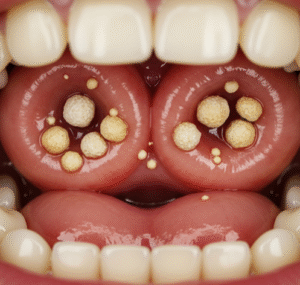
- Swollen lymph nodes or neurological symptoms in extrapulmonary TB
- Digestive problems in gastrointestinal TB
Early detection in Korean healthcare facilities is crucial to prevent severe complications and limit transmission.
Causes
TB is caused by infection with Mycobacterium tuberculosis. Transmission occurs when inhaling airborne droplets containing the bacteria. Factors contributing to TB infection and progression include:
- Close contact with an individual with active pulmonary TB
- Weakened immune system due to HIV infection, chronic illness, or immunosuppressive therapy
- Malnutrition, smoking, or alcohol abuse that compromise immunity
- Poor living conditions or overcrowding, which facilitate airborne transmission
- Previous TB exposure or latent infection that reactivates later
Understanding these causes helps Korean public health authorities implement effective screening, vaccination, and preventive measures.
Risk Factors
Certain factors increase susceptibility to TB:
- Immunodeficiency, including HIV infection or long-term corticosteroid use
- Diabetes or other chronic medical conditions
- Advanced age or very young age
- Close living quarters or frequent contact with TB patients
- Malnutrition or lifestyle factors affecting immune health
South Korean health programs prioritize high-risk populations for TB screening, vaccination, and monitoring.
Complications
If left untreated, TB can lead to serious health complications:
- Pulmonary complications: Chronic lung damage, cavitation, respiratory failure
- Extrapulmonary TB: Infection of lymph nodes, bones (Pott’s disease), kidneys, or brain (tuberculous meningitis)
- Miliary TB: Widespread infection affecting multiple organs, potentially life-threatening
- Drug-resistant TB: Multidrug-resistant TB (MDR-TB) or extensively drug-resistant TB (XDR-TB) requiring longer, complex treatment
- Malnutrition and weight loss: Due to chronic illness
- Transmission to others: Active pulmonary TB is highly contagious
Early intervention in South Korea significantly reduces the risk of these complications and limits community spread.
Prevention
TB prevention focuses on reducing transmission and protecting high-risk populations:
- BCG vaccination: Administered to newborns to protect against severe forms of TB
- Screening programs: Routine chest X-rays and TB tests for high-risk individuals, healthcare workers, and contacts of TB patients
- Infection control measures: Masking, isolation, and proper ventilation in healthcare settings
- Prompt treatment of latent TB: Reduces progression to active disease
- Public education: Awareness campaigns about TB symptoms, transmission, and adherence to treatment
South Korea’s national TB control strategy combines vaccination, surveillance, and public health education to reduce incidence and mortality.
Treatment Options in Korea
TB treatment in South Korea is highly standardized and effective when patients adhere to prescribed regimens:
Diagnosis:
- Sputum smear microscopy, culture tests, and nucleic acid amplification tests for pulmonary TB
- Imaging studies (chest X-ray or CT scan) to detect lung involvement
- Blood tests and biopsies for extrapulmonary TB
- Drug susceptibility testing to identify resistant strains
Medical Treatments:
- First-line antibiotics: Combination therapy with isoniazid, rifampicin, ethambutol, and pyrazinamide for 6–9 months
- Second-line therapy: For MDR-TB or XDR-TB, using longer, more complex regimens with newer or second-line drugs
- Directly observed therapy (DOT): Ensures adherence to treatment and prevents resistance
Supportive Care:
- Nutritional support to improve immunity and recovery
- Management of side effects, such as liver toxicity or gastrointestinal issues
- Counseling and monitoring for mental health due to prolonged treatment
- Rehabilitation for lung function in severe cases
South Korean healthcare facilities integrate advanced diagnostics, effective pharmacological treatment, and comprehensive public health measures to ensure TB is managed effectively, reducing mortality and preventing transmission.