Overview
Trichotillomania is a psychological disorder characterized by the recurrent, irresistible urge to pull out one’s own hair, leading to noticeable hair loss and significant distress or functional impairment. Classified under obsessive-compulsive and related disorders, trichotillomania can affect the scalp, eyebrows, eyelashes, or other body hair. In South Korea, mental health professionals, including psychiatrists, psychologists, and dermatologists, provide integrated care involving behavioral therapy, pharmacologic interventions, and support groups. Early recognition and treatment are crucial to reduce hair loss, prevent skin damage, and improve overall mental health and quality of life.
What is Trichotillomania?
Trichotillomania, sometimes called hair-pulling disorder, involves repetitive hair-pulling behaviors that individuals feel unable to control. These urges often increase during periods of stress, anxiety, or boredom. Hair pulling may be conscious (focused) or automatic (habitual without awareness). Over time, repeated pulling can result in bald patches, scarring, and social embarrassment. In Korea, specialists utilize diagnostic criteria from the DSM-5 and employ clinical interviews, behavioral assessments, and sometimes dermatologic evaluations to confirm the diagnosis.
Symptoms
Symptoms of trichotillomania can vary in severity and may include:
- Recurrent hair pulling from the scalp, eyebrows, eyelashes, or other body areas
- Noticeable hair loss or thinning patches
- Repetitive behaviors such as twisting, twirling, or biting pulled hair
- Difficulty controlling the urge to pull hair despite attempts to stop
- Distress, shame, or anxiety related to hair loss
- Social withdrawal or avoidance of public settings
- Skin irritation, redness, or scarring in areas of frequent hair pulling
- In severe cases, complications such as infections or gastrointestinal issues from swallowing hair (trichophagia)
Korean mental health clinics emphasize careful observation and patient self-reporting to identify patterns and triggers.
Causes
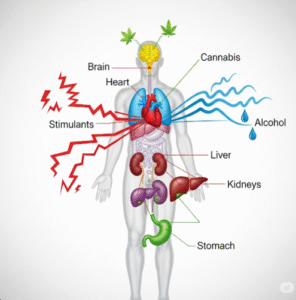
The exact cause of trichotillomania is not fully understood, but several factors contribute to its development:
- Genetic predisposition: Family history of obsessive-compulsive or related disorders
- Neurological factors: Differences in brain chemistry affecting impulse control
- Psychological factors: Anxiety, stress, depression, or traumatic experiences
- Behavioral conditioning: Repeated hair pulling may provide temporary relief from tension or emotional discomfort
- Environmental triggers: High-stress situations or certain social pressures
Korean researchers and clinicians adopt a biopsychosocial approach, considering genetic, neurological, psychological, and environmental influences when developing treatment plans.
Risk Factors
Several factors may increase the likelihood of developing trichotillomania:
- Female gender, as the disorder is more prevalent among women
- Childhood or adolescence, which is the typical age of onset
- Coexisting mental health conditions such as anxiety, depression, or OCD
- Family history of related psychiatric disorders
- High-stress environments or exposure to traumatic events
Early recognition of risk factors in Korea allows mental health professionals to intervene before the disorder causes severe hair loss or psychosocial complications.
Complications
Trichotillomania can lead to multiple physical, emotional, and social complications:
- Permanent hair loss or patchy baldness
- Skin damage, infections, or scarring from repeated pulling
- Trichophagia (ingesting hair), which can lead to hairballs (trichobezoars) in the gastrointestinal tract
- Low self-esteem, social anxiety, or depression
- Interpersonal difficulties and social withdrawal
- Impaired academic or work performance due to distress or preoccupation with hair pulling
Mental health support in South Korea focuses on addressing both the behavioral and emotional aspects of the disorder to minimize these complications.
Prevention
While trichotillomania cannot always be fully prevented, certain strategies may help reduce onset or recurrence:
- Stress management through relaxation techniques, mindfulness, or meditation
- Early recognition and intervention in children or adolescents exhibiting hair-pulling behaviors
- Supportive family or social environments
- Cognitive-behavioral strategies to develop alternative coping mechanisms
- Monitoring for coexisting mental health conditions and addressing them promptly
Korean mental health programs emphasize education and early intervention to minimize the disorder’s impact on daily life.
Treatment Options in Korea
Treatment of trichotillomania in Korea involves a combination of behavioral therapy, pharmacologic intervention, and supportive care:
Diagnosis:
- Clinical assessment by psychiatrists or psychologists using DSM-5 criteria
- Behavioral and psychological evaluation to identify triggers and patterns
- Dermatologic assessment for hair loss and skin health
Behavioral Treatments:
- Cognitive Behavioral Therapy (CBT): Focused on changing thoughts and behaviors related to hair pulling
- Habit Reversal Training (HRT): Teaches patients to replace hair-pulling urges with alternative behaviors
- Mindfulness and stress-reduction techniques: To manage emotional triggers
- Support groups and psychoeducation: Encourage peer support and coping strategies
Pharmacologic Treatments:
- Selective Serotonin Reuptake Inhibitors (SSRIs): To manage coexisting anxiety or depressive symptoms
- N-acetylcysteine: Sometimes used to reduce compulsive urges
- Other medications: Prescribed based on individual needs and psychiatric evaluation
Supportive Care:
- Family counseling and education on how to support the patient
- Skin care management for areas affected by hair pulling
- Ongoing monitoring to prevent relapse and track progress
- Integration of multidisciplinary teams including psychiatrists, psychologists, and dermatologists
Korean mental health centers combine modern psychiatric care, behavioral interventions, and patient-centered support to optimize recovery and improve long-term outcomes.