Overview
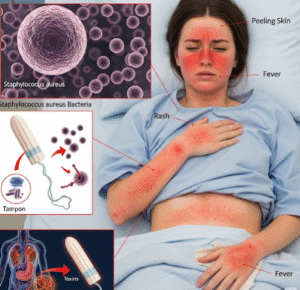
Toxic Shock Syndrome (TSS) is a rare but life-threatening condition caused by toxins produced by certain strains of bacteria, most commonly Staphylococcus aureus and Streptococcus pyogenes. TSS can develop rapidly and affect multiple organ systems, leading to shock, organ failure, and, if untreated, death. In South Korea, advanced hospitals and infectious disease specialists provide prompt diagnosis, intensive care, and antibiotic therapy to manage TSS effectively. Public health education also focuses on early recognition, hygienic practices, and proper management of risk factors to prevent severe outcomes.
What is Toxic Shock Syndrome (TSS)?
Toxic Shock Syndrome is a systemic illness triggered by bacterial toxins that enter the bloodstream and cause an exaggerated immune response. These toxins act as superantigens, overstimulating the immune system and leading to widespread inflammation. TSS can occur in various contexts, including menstrual-associated cases (linked to tampon use), postoperative infections, skin wounds, and soft tissue infections. In Korea, physicians emphasize rapid identification and aggressive treatment, as the condition can progress within hours.
Symptoms
TSS symptoms develop quickly and often involve multiple organ systems. Key signs include:
- Sudden high fever (often above 38.9°C / 102°F)
- Hypotension (low blood pressure) leading to dizziness or fainting
- Rash resembling a sunburn, particularly on the palms and soles
- Redness of eyes, mouth, and throat
- Nausea, vomiting, and diarrhea
- Muscle aches and severe weakness
- Confusion or altered mental status
- Organ involvement, including kidney or liver dysfunction in severe cases
In menstrual-associated TSS, symptoms typically occur during or shortly after tampon use, whereas non-menstrual TSS may follow surgery, injury, or skin infections.
Causes
TSS is caused by bacterial toxins entering the bloodstream. Major causes include:
- Staphylococcus aureus toxins: Often linked to prolonged tampon use, nasal packing, or wound infections
- Streptococcus pyogenes toxins: Associated with skin wounds, burns, or post-surgical infections
- Postoperative infections: Surgical sites can provide an entry point for bacteria
- Skin injuries: Cuts, burns, or insect bites that become contaminated
- Use of foreign materials: Tampons, contraceptive sponges, or wound dressings that promote bacterial growth
Korean infectious disease specialists carefully evaluate the source of infection to guide treatment and prevent recurrence.
Risk Factors
Certain factors increase the likelihood of developing TSS:
- Women using high-absorbency tampons for extended periods
- Surgical procedures or postoperative wounds
- Skin injuries, burns, or abrasions
- Pre-existing infections or chronic skin conditions
- Immunosuppressive therapy or weakened immune system
- Young age, particularly menstruating women and children
- Recent viral infections that may predispose the body to bacterial overgrowth
Public awareness campaigns in Korea educate high-risk populations on early signs and preventive measures.
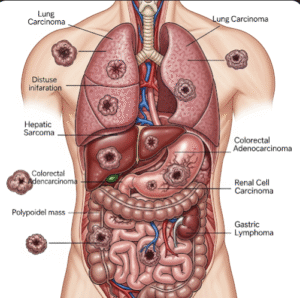
Complications
If left untreated, TSS can lead to severe complications:
- Shock and dangerously low blood pressure
- Multi-organ failure, including kidney, liver, and heart complications
- Respiratory distress requiring mechanical ventilation
- Blood clotting disorders and disseminated intravascular coagulation
- Long-term organ damage or neurological deficits
- Death in severe, untreated cases
Rapid intervention in Korean hospitals significantly reduces mortality and long-term complications.
Prevention
Preventive strategies for TSS focus on hygiene, awareness, and careful management of risk factors:
- Tampon use: Use the lowest absorbency necessary, change frequently, and alternate with pads
- Wound care: Keep cuts, abrasions, and surgical sites clean and properly dressed
- Prompt treatment of infections: Seek early medical care for skin, respiratory, or systemic infections
- Avoid prolonged use of foreign materials: Nasal packing, contraceptive sponges, or dressings
- Monitor for early symptoms: Fever, rash, or malaise in the context of risk factors
- Educate high-risk populations: Women, post-surgical patients, and caregivers on TSS signs
In South Korea, public health programs emphasize education on hygiene, tampon safety, and early medical consultation.
Treatment Options in Korea
Treatment of TSS in Korea is urgent and multidisciplinary, often involving intensive care:
Diagnosis:
- Rapid clinical assessment for fever, rash, hypotension, and multi-organ involvement
- Blood tests, including complete blood count, renal and liver function tests
- Blood cultures to identify causative bacteria
- Imaging studies if a localized infection source is suspected
Medical Treatments:
- Antibiotics: Intravenous therapy targeting Staphylococcus aureus or Streptococcus pyogenes
- Intravenous fluids: To maintain blood pressure and support organ function
- Vasopressors: For patients with severe hypotension
- Supportive care: Oxygen therapy, mechanical ventilation, or dialysis if organs are affected
- Surgical intervention: Drainage of abscesses or removal of infected tissue if necessary
Supportive Care:
- Monitoring in an intensive care unit for severe cases
- Pain management and fever control
- Regular assessment for organ function and potential complications
- Patient education on wound care and hygiene after discharge
South Korean hospitals integrate rapid diagnosis, targeted antibiotic therapy, and advanced supportive care to improve survival rates and minimize complications from TSS.