Overview
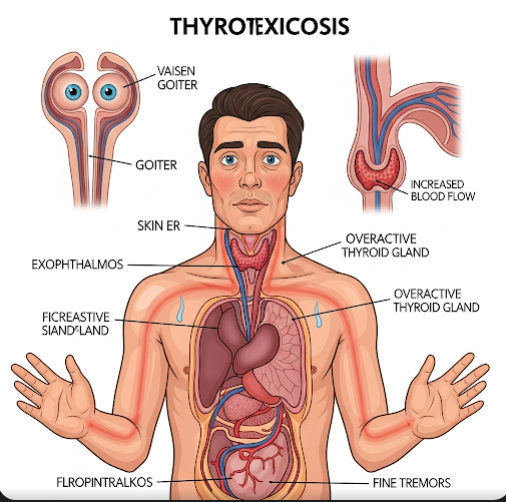
Thyrotoxicosis is a clinical condition characterized by an excess of thyroid hormones in the bloodstream, leading to an acceleration of the body’s metabolic processes. It can arise from various thyroid disorders, including hyperthyroidism, thyroiditis, or excessive intake of thyroid hormone medication. In South Korea, thyrotoxicosis is recognized as a significant endocrine disorder, and patients benefit from advanced diagnostic tools, effective medical management, and ongoing monitoring. Korean healthcare providers emphasize early detection, precise diagnosis, and comprehensive treatment to prevent complications and improve patient quality of life.
What is Thyrotoxicosis?
Thyrotoxicosis refers to the state of having abnormally high levels of thyroid hormones—thyroxine (T4) and triiodothyronine (T3)—in the body. While often used interchangeably with hyperthyroidism, thyrotoxicosis encompasses any cause of excess circulating thyroid hormones, including thyroid inflammation (thyroiditis) or exogenous hormone intake. The excess hormones accelerate metabolism, affecting multiple organ systems, including the heart, nervous system, gastrointestinal tract, and musculoskeletal system. In Korea, endocrinologists utilize laboratory testing, imaging, and clinical evaluation to differentiate the underlying causes and guide treatment.
Symptoms
Symptoms of thyrotoxicosis vary depending on the severity and underlying cause but commonly include:
- Unexplained weight loss despite normal or increased appetite
- Rapid or irregular heartbeat (palpitations)
- Nervousness, anxiety, or irritability
- Tremors in hands and fingers
- Excessive sweating and heat intolerance
- Increased bowel movements or diarrhea
- Fatigue or muscle weakness
- Sleep disturbances or insomnia
- Goiter or swelling in the neck in cases of hyperthyroidism
- Eye changes, such as bulging eyes, in Graves’ disease-related thyrotoxicosis
Early recognition of these symptoms in South Korea allows for timely intervention and prevention of severe complications.
Causes
Thyrotoxicosis can result from various conditions, including:
- Graves’ disease: Autoimmune disorder causing overstimulation of the thyroid
- Toxic multinodular goiter: Multiple overactive thyroid nodules
- Thyroid adenoma: Single overactive nodule
- Thyroiditis: Inflammation of the thyroid gland causing hormone leakage
- Excess thyroid hormone intake: Overmedication or dietary supplements
- Postpartum thyroiditis: Temporary hormone excess after childbirth
Korean healthcare providers assess the underlying cause through blood tests, antibody studies, and imaging to ensure targeted treatment.
Risk Factors
Several factors increase the likelihood of developing thyrotoxicosis:
- Female gender, particularly between 20 and 40 years of age
- Family history of thyroid disease or autoimmune disorders
- Personal history of autoimmune conditions, such as type 1 diabetes or rheumatoid arthritis
- Pregnancy or postpartum period
- Iodine supplementation or exposure to high iodine intake
- Stress or severe illness, which can trigger thyroid inflammation
Identifying risk factors in Korea allows clinicians to monitor high-risk patients closely and implement preventive strategies.
Complications
If left untreated, thyrotoxicosis can lead to significant complications:
- Cardiovascular issues: Arrhythmia, atrial fibrillation, high blood pressure, or heart failure
- Osteoporosis: Accelerated bone loss due to high metabolic activity
- Muscle weakness and fatigue: Leading to reduced mobility
- Thyroid storm: A rare, life-threatening exacerbation with fever, severe tachycardia, and multi-organ dysfunction
- Eye problems: In cases of Graves’ disease, including vision impairment or corneal damage
- Psychological effects: Anxiety, depression, or mood disturbances
Korean healthcare facilities emphasize early treatment and careful monitoring to prevent these severe outcomes.
Prevention
While not all causes of thyrotoxicosis are preventable, certain measures can reduce risk and aid early detection:
- Regular thyroid checkups: Especially for individuals with family history or autoimmune disorders
- Balanced iodine intake: Avoiding excessive supplementation
- Monitoring thyroid hormone therapy: Ensuring correct dosages in patients receiving treatment
- Awareness of early symptoms: Prompt consultation with endocrinologists for palpitations, weight loss, or tremors
- Management of autoimmune conditions: Reducing triggers that may exacerbate thyroid dysfunction
South Korean public health initiatives and specialized endocrinology clinics provide education to improve awareness and early intervention.
Treatment Options in Korea
Treatment of thyrotoxicosis in Korea is tailored according to the underlying cause, patient condition, and severity:
Diagnosis:
- Blood tests measuring TSH, T3, and T4 levels
- Thyroid antibody testing for autoimmune causes
- High-resolution ultrasound or scintigraphy to assess gland structure and activity
- Electrocardiogram (ECG) and heart monitoring in cases with cardiac symptoms
Medical Treatments:
- Antithyroid medications: Methimazole or propylthiouracil to inhibit hormone production
- Beta-blockers: To manage symptoms like palpitations, tremors, and anxiety
- Radioactive iodine therapy: To reduce thyroid activity in hyperthyroidism
- Surgery (thyroidectomy): Reserved for severe, recurrent, or structural causes, such as large goiters or nodules
Supportive Care:
- Regular follow-up to monitor hormone levels and adjust treatment
- Nutritional guidance to maintain bone health and overall metabolism
- Management of cardiovascular symptoms and anxiety
- Education on early warning signs of thyroid storm and when to seek emergency care
Korean hospitals offer a multidisciplinary approach, combining endocrinologists, cardiologists, nutritionists, and surgeons to ensure comprehensive care, minimize complications, and improve patient quality of life.