Overview
Thyrotoxicosis is a clinical condition resulting from excess thyroid hormones circulating in the body, leading to hypermetabolic symptoms and systemic effects. It can arise from a variety of thyroid disorders, including Graves’ disease, toxic multinodular goiter, and overactive thyroid nodules. If left untreated, thyrotoxicosis can cause severe complications such as heart failure, osteoporosis, and thyrotoxic crisis (thyroid storm). South Korea offers advanced diagnostic tools and treatment options, combining endocrinology, nuclear medicine, and minimally invasive surgery to manage thyrotoxicosis effectively and safely.
What is Thyrotoxicosis?
Thyrotoxicosis is not a disease in itself but a syndrome caused by elevated levels of thyroid hormones (T3 and T4) in the bloodstream. These hormones regulate metabolism, energy levels, and various organ functions. Excess thyroid hormones accelerate metabolic processes, leading to symptoms such as rapid heartbeat, weight loss, heat intolerance, and nervous system hyperactivity.
Common causes of thyrotoxicosis include:
- Graves’ disease: Autoimmune stimulation of the thyroid leading to excessive hormone production.
- Toxic multinodular goiter: Multiple nodules in the thyroid producing hormones independently of regulatory signals.
- Thyroid adenomas: Benign tumors that secrete excess thyroid hormones.
- Thyroiditis: Inflammation of the thyroid gland causing hormone release.
- Excessive intake of thyroid hormones: Often due to overmedication in hypothyroid patients.
Symptoms
The symptoms of thyrotoxicosis are primarily related to the hypermetabolic effects of excess thyroid hormones:
Cardiovascular symptoms:
- Rapid heartbeat (tachycardia)
- Palpitations or irregular heartbeat (arrhythmia)
- High blood pressure
- Shortness of breath during physical activity
Neurological and psychological symptoms:
- Anxiety, nervousness, or irritability
- Tremors, particularly in hands and fingers
- Sleep disturbances
- Difficulty concentrating
Systemic symptoms:
- Unintended weight loss despite normal or increased appetite
- Heat intolerance and excessive sweating
- Muscle weakness or fatigue
- Increased bowel movements or diarrhea
- Hair thinning and brittle nails
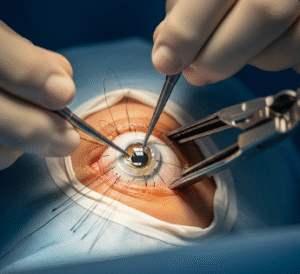
Ocular symptoms (if associated with Graves’ disease):
- Bulging eyes (proptosis)
- Redness or irritation
- Double vision
Early recognition of these symptoms is crucial to prevent progression to severe complications.
Causes
Thyrotoxicosis results from an excess of thyroid hormones due to a variety of conditions:
- Autoimmune hyperthyroidism: Graves’ disease is the most common cause worldwide.
- Overactive thyroid nodules: Autonomous nodules produce hormones independently.
- Thyroid inflammation: Subacute thyroiditis or silent thyroiditis can release stored hormones.
- Excessive hormone intake: Overuse of levothyroxine or other thyroid medications.
- Medications: Certain drugs such as amiodarone can induce thyrotoxicosis.
- Postpartum thyroid disorders: Autoimmune flare-ups after pregnancy may trigger hormone excess.
Risk Factors
Certain factors increase the risk of developing thyrotoxicosis:
- Female gender, particularly with autoimmune predispositions
- Age between 20 and 50 years
- Family history of thyroid disorders
- History of autoimmune diseases such as type 1 diabetes or lupus
- Smoking, which increases severity of associated eye disease
- Previous thyroid surgery or radiation exposure
Complications
Untreated thyrotoxicosis can lead to severe and potentially life-threatening complications:
- Heart complications: Atrial fibrillation, heart failure, or angina
- Osteoporosis: Accelerated bone loss due to hormone excess
- Thyroid storm: Acute, life-threatening exacerbation of hyperthyroidism
- Eye complications: Severe proptosis and optic nerve damage in Graves’ orbitopathy
- Metabolic disturbances: Severe weight loss, electrolyte imbalance, and dehydration
Early diagnosis and management in Korean medical centers significantly reduce the risk of these complications.
Prevention
Prevention of thyrotoxicosis focuses on controlling underlying thyroid disorders and avoiding triggers:
- Adhere strictly to prescribed thyroid medications
- Regular monitoring of thyroid hormone levels and antibody titers
- Prompt treatment of infections or illnesses that can exacerbate hyperthyroidism
- Avoid excessive iodine intake, which can precipitate hormone overproduction
- Lifestyle modifications, including stress management and smoking cessation
- Preoperative stabilization before surgery for patients with known hyperthyroidism
Treatment Options in Korea
South Korea provides advanced, multidisciplinary treatment for thyrotoxicosis, ensuring both symptom control and long-term disease management.
Diagnosis:
- Comprehensive thyroid function tests (T3, T4, TSH)
- Blood tests for thyroid antibodies
- Ultrasound and Doppler studies to assess nodules or gland vascularity
- Radioactive iodine uptake scans to identify areas of overactivity
- Electrocardiogram (ECG) and echocardiography for cardiovascular assessment
Medical Treatments:
- Anti-thyroid drugs: Methimazole or propylthiouracil to reduce hormone production
- Beta-blockers: Control heart rate, tremors, and anxiety
- Corticosteroids: For severe inflammation, particularly with eye involvement
- Supportive care: Nutritional guidance, hydration, and management of electrolyte imbalance
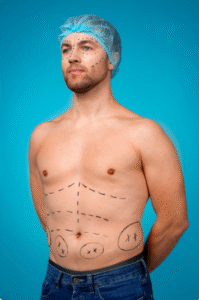
Surgical or Advanced Therapies:
- Thyroidectomy: Partial or total removal of the thyroid in resistant or high-risk cases
- Radioactive iodine therapy: Destroys overactive thyroid tissue to restore hormonal balance
- Minimally invasive and robotic-assisted surgery: Available in leading Korean hospitals for faster recovery and reduced scarring
Rehabilitation and Support:
- Regular monitoring of thyroid function and hormone replacement if needed
- Eye care management for patients with associated orbitopathy
- Lifestyle counseling to reduce recurrence and maintain thyroid health
- Psychological support for patients dealing with chronic symptoms or cosmetic concerns
Korean hospitals excel in combining endocrinology, nuclear medicine, and surgery to provide a patient-centered approach that ensures rapid symptom relief, long-term disease control, and minimal complications.