Overview
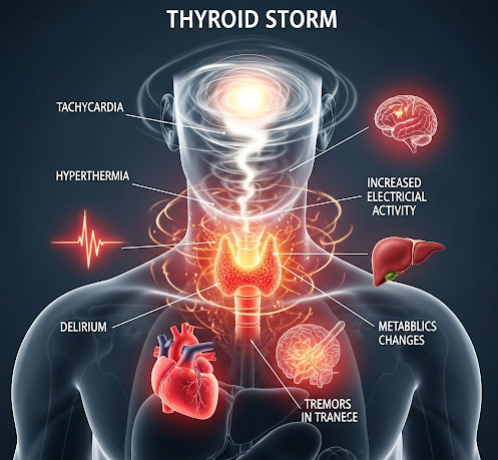
Thyroid storm is a rare but life-threatening complication of hyperthyroidism, characterized by an extreme overproduction of thyroid hormones. This condition represents a medical emergency, as it can rapidly affect multiple organ systems, including the heart, liver, and nervous system. Prompt recognition and treatment are critical to prevent serious complications or death. South Korea is renowned for its advanced endocrine care and critical care facilities, offering rapid diagnosis, intensive management, and specialized treatment for patients experiencing thyroid storm. Early intervention in Korea’s medical centers can significantly improve outcomes and reduce mortality rates.
What is Thyroid Storm?
Thyroid storm, also called thyrotoxic crisis, occurs when the body experiences an acute surge of thyroid hormones, leading to exaggerated symptoms of hyperthyroidism. It often develops in patients with untreated or poorly controlled hyperthyroidism, particularly Graves’ disease. Triggers can include infection, surgery, trauma, or discontinuation of anti-thyroid medications. Unlike typical hyperthyroidism, thyroid storm presents with severe systemic effects and requires immediate hospitalization. Without prompt treatment, it can progress to multi-organ failure.
Symptoms
Thyroid storm presents with sudden and severe symptoms, often affecting multiple organ systems:
Cardiovascular symptoms:
- Rapid heartbeat (tachycardia)
- Irregular heartbeat (arrhythmia)
- High blood pressure initially, followed by low blood pressure in severe cases
- Heart failure
Neurological symptoms:
- Agitation, confusion, or delirium
- Tremors
- Seizures in extreme cases
Systemic and metabolic symptoms:
- High fever, often above 38.5°C (101.3°F)
- Profuse sweating
- Severe weakness or fatigue
- Unexplained weight loss
- Nausea, vomiting, and diarrhea
Ocular and other symptoms:
- Eye irritation or bulging (if associated with Graves’ disease)
- Dehydration due to excessive fluid loss
- Potential liver dysfunction
Early recognition of these symptoms is critical, as thyroid storm can deteriorate rapidly without treatment.
Causes
Thyroid storm usually occurs in patients with existing hyperthyroidism and can be triggered by factors that increase thyroid hormone levels or exacerbate their effects:
- Infections: Respiratory infections or sepsis can precipitate a storm.
- Surgery or trauma: Physical stress can trigger excessive hormone release.
- Medication noncompliance: Stopping anti-thyroid drugs suddenly.
- Acute illness: Heart attack, stroke, or diabetic ketoacidosis.
- Radioactive iodine therapy: Occasionally triggers a storm in susceptible patients.
- Severe hyperthyroidism: Uncontrolled Graves’ disease or toxic multinodular goiter.
Risk Factors
Certain patients are more susceptible to developing thyroid storm:
- Individuals with untreated or poorly controlled hyperthyroidism
- Elderly patients with underlying cardiovascular disease
- Patients undergoing major surgery without proper thyroid stabilization
- Infections or other acute medical conditions
- History of previous thyroid storm
- Women, particularly during postpartum periods, due to increased risk of thyroid fluctuations
Complications
Thyroid storm is a critical emergency with potentially fatal complications if not treated promptly:
- Heart failure: Severe tachycardia or arrhythmias can lead to cardiac collapse.
- Multi-organ failure: Including liver, kidney, and respiratory dysfunction.
- Shock: Low blood pressure and poor perfusion can occur.
- Neurological damage: Delirium, seizures, or coma.
- Death: Mortality rates remain high without immediate intensive care.
Early recognition and intensive treatment in specialized Korean hospitals greatly reduce these risks.
Prevention
Preventing thyroid storm focuses on controlling hyperthyroidism and avoiding known triggers:
- Adherence to anti-thyroid medications as prescribed
- Regular monitoring of thyroid hormone levels
- Stabilization of thyroid function before surgery or invasive procedures
- Prompt treatment of infections and acute illnesses
- Patient education about warning signs and risk factors
- Avoid abrupt discontinuation of medications
Treatment Options in Korea
South Korea provides advanced and multidisciplinary management of thyroid storm, integrating endocrinology, critical care, and surgical expertise.
Diagnosis:
- Rapid assessment of vital signs and systemic symptoms
- Laboratory tests to confirm thyroid hormone levels (T3, T4, TSH)
- Assessment of liver and kidney function
- Electrocardiogram (ECG) to detect arrhythmias
- Imaging if complications such as heart failure or pulmonary edema are suspected
Medical Treatments:
- Anti-thyroid medications: Propylthiouracil (PTU) or methimazole to block hormone production
- Beta-blockers: To control heart rate, reduce tremors, and manage cardiovascular stress
- Corticosteroids: Reduce peripheral conversion of T4 to T3 and decrease inflammation
- Supportive care: Intravenous fluids, electrolytes, and oxygen as needed
- Temperature management: Cooling measures for high fever
Surgical or Advanced Therapies:
- Thyroidectomy: Considered once the patient is stabilized if the underlying cause is a toxic nodule or goiter
- Radioactive iodine therapy: Post-stabilization in select cases of hyperthyroidism
Rehabilitation and Support:
- Continuous monitoring in intensive care units until stable
- Long-term management of hyperthyroidism to prevent recurrence
- Nutritional and lifestyle counseling to maintain thyroid balance
- Patient education on early warning signs for rapid intervention
South Korea’s hospitals are equipped with modern intensive care units, endocrinology specialists, and multidisciplinary teams, making early recognition and aggressive treatment of thyroid storm highly effective.