Overview
Thalassaemia is a group of inherited blood disorders characterized by abnormal hemoglobin production, leading to reduced red blood cell formation and chronic anemia. The condition ranges from mild forms, which may be asymptomatic, to severe forms requiring lifelong medical care. In South Korea, advanced hematology and genetic testing facilities provide comprehensive diagnosis, treatment, and genetic counseling for individuals with thalassaemia. The country’s healthcare system emphasizes early detection, personalized management plans, and supportive therapies to improve quality of life and prevent complications associated with the disease.
What is Thalassaemia?
Thalassaemia results from genetic mutations affecting the alpha or beta globin chains of hemoglobin, the protein responsible for carrying oxygen in red blood cells. Depending on which chain is affected, thalassaemia is classified as:
- Alpha thalassaemia: Caused by mutations in the alpha-globin genes
- Beta thalassaemia: Caused by mutations in the beta-globin genes
The severity of the disorder depends on the number and type of genes affected. Severe forms, such as beta-thalassaemia major, can result in life-threatening anemia, while milder forms, like thalassaemia minor, may cause only mild symptoms or be asymptomatic. Korean medical centers specialize in genetic testing to accurately classify the type and severity, enabling tailored treatment strategies.
Symptoms
Symptoms of thalassaemia vary based on the type and severity of the disorder:
- Chronic fatigue and weakness due to anemia
- Pale or yellowish skin (jaundice)
- Slow growth or delayed puberty in children
- Bone deformities, particularly in the face and skull
- Enlarged spleen (splenomegaly) and liver (hepatomegaly)
- Shortness of breath and dizziness
- Dark urine from increased red blood cell breakdown
- Frequent infections due to compromised immunity in severe cases
Early recognition of symptoms allows Korean hematologists to intervene promptly and prevent long-term complications.
Causes
Thalassaemia is an inherited genetic disorder caused by mutations in the genes responsible for hemoglobin production. It is passed down from parents to children through autosomal recessive inheritance:
- Both parents carrying the mutated gene can pass the condition to their offspring
- Alpha or beta globin gene mutations reduce or eliminate normal hemoglobin production
- Environmental factors do not cause thalassaemia, but inadequate treatment can exacerbate complications
In South Korea, genetic counseling services help families understand the risk of inheritance and plan for appropriate interventions.
Risk Factors
Risk factors for thalassaemia are primarily genetic:
- Family history of thalassaemia or carrier status
- Ethnic background, with higher prevalence in Mediterranean, Middle Eastern, South Asian, and Southeast Asian populations
- Consanguinity or marriage between closely related individuals increasing the risk of inheriting the disorder
- Parental carriers of thalassaemia minor may have a child with thalassaemia major
Korean clinics offer pre-marital and prenatal genetic screening to identify carriers and reduce the risk of severe forms of the disease.
Complications
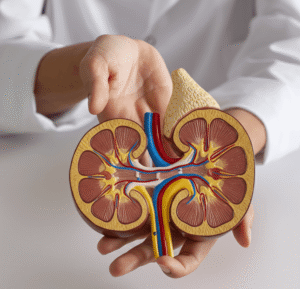
Untreated or poorly managed thalassaemia can lead to serious complications:
- Severe anemia requiring frequent blood transfusions
- Iron overload due to repeated transfusions, affecting the heart, liver, and endocrine glands
- Bone deformities and growth retardation
- Enlarged spleen and liver, leading to organ dysfunction
- Increased susceptibility to infections
- Heart failure or liver disease from iron accumulation
- Psychological and social challenges due to chronic illness
Early diagnosis and comprehensive treatment in Korea help minimize these complications and improve long-term outcomes.
Prevention
While thalassaemia cannot be entirely prevented due to its genetic origin, several strategies can reduce the incidence and impact:
- Genetic counseling: Advising at-risk couples about inheritance patterns and reproductive options
- Prenatal screening: Identifying affected fetuses for early intervention or informed decision-making
- Carrier screening programs: Detecting thalassaemia carriers before pregnancy
- Public awareness campaigns: Educating communities about genetic testing and preventive strategies
- Blood donation and transfusion safety: Ensuring safe transfusion practices to manage anemia
Korean medical centers provide comprehensive programs combining genetic counseling, prenatal testing, and public education to mitigate the disease burden.
Treatment Options in Korea
Treatment of thalassaemia in South Korea is tailored to the severity of the disorder and includes medical management, supportive care, and advanced therapies:
Diagnosis:
- Blood tests to detect anemia and abnormal hemoglobin
- Hemoglobin electrophoresis to identify specific hemoglobin variants
- Genetic testing to classify alpha or beta thalassaemia and predict severity
- Imaging studies for spleen and liver assessment
Medical Treatments:
- Regular blood transfusions: Essential for patients with severe thalassaemia to maintain healthy hemoglobin levels
- Iron chelation therapy: Medications such as deferoxamine or deferasirox to prevent iron overload from repeated transfusions
- Folic acid supplements: Support red blood cell production
Advanced Therapies:
- Bone marrow or stem cell transplantation: Potential curative treatment for eligible patients
- Gene therapy: Experimental approaches to correct defective hemoglobin genes
- Supportive care: Management of complications such as heart or liver disease, bone deformities, and growth delays
Lifestyle and Support:
- Nutritional guidance to support overall health
- Regular monitoring of iron levels and organ function
- Psychological support and patient education to manage chronic illness
South Korea’s healthcare system integrates hematology specialists, genetic counselors, and advanced treatment facilities to provide comprehensive care for individuals with thalassaemia, ensuring improved quality of life and long-term survival.