Overview
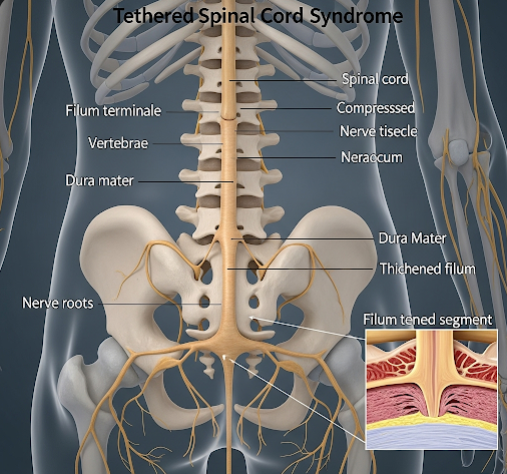
Tethered Spinal Cord Syndrome (TSCS) is a neurological disorder in which the spinal cord is abnormally attached or “tethered” to surrounding tissues, restricting its movement within the spinal column. This abnormal attachment can cause stretching of the spinal cord as a child grows or due to spinal trauma, leading to neurological symptoms. TSCS can be congenital (present at birth) or acquired, and early diagnosis is critical to prevent permanent nerve damage. In Korea, specialized neurosurgical centers and advanced imaging technologies provide comprehensive care, including accurate diagnosis, minimally invasive surgery, and long-term rehabilitation.
What is Tethered Spinal Cord Syndrome?
Tethered Spinal Cord Syndrome occurs when the spinal cord is abnormally fixed to tissues such as fibrous bands, fatty deposits, or scar tissue, limiting its normal movement. Normally, the spinal cord moves freely within the spinal canal, adjusting with growth and body movements. In TSCS, the tethering can cause tension on the spinal cord, leading to neurological dysfunction. This condition can present at any age but is often identified in children when growth accelerates.
Symptoms
Symptoms of TSCS vary depending on age, severity, and location of the tethered cord. Common signs include:
- Back pain or lower back stiffness
- Leg pain, weakness, or numbness
- Difficulty walking or changes in gait
- Loss of bladder or bowel control
- Scoliosis or abnormal spinal curvature
- Muscle spasms or abnormal reflexes
- Fatigue or discomfort during prolonged standing or activity
In infants or young children, symptoms may be subtle, such as delayed motor milestones, foot deformities, or skin abnormalities over the lower back. Adults may develop progressive neurological deficits if TSCS is not treated.
Causes
Tethered Spinal Cord Syndrome can be caused by several factors:
- Congenital malformations: Most cases are associated with spina bifida, lipomyelomeningocele, or other spinal dysraphisms.
- Scar tissue or adhesions: Post-surgical or post-traumatic scarring can tether the spinal cord.
- Fatty tumors (lipomas): Lipomas can attach to the spinal cord, causing tension.
- Trauma: Injuries to the spine may result in acquired tethering.
- Spinal tumors: Rarely, tumors may anchor the spinal cord.
Risk Factors
Certain factors increase the risk of TSCS:
- Congenital spinal defects: Children born with spina bifida or related conditions
- Previous spinal surgery or trauma: Scar tissue formation may tether the cord
- Rapid growth in children: Tethered cord symptoms often emerge during growth spurts
- Genetic factors: Some congenital spinal abnormalities may have hereditary components
Complications
If left untreated, TSCS can lead to severe and permanent complications:
- Progressive neurological deficits, including paralysis of lower limbs
- Permanent bladder and bowel dysfunction
- Chronic pain and mobility limitations
- Scoliosis and other spinal deformities
- Sensory deficits in the lower extremities
- Muscle weakness or atrophy due to prolonged nerve tension
- Reduced quality of life due to chronic disability
Prevention
While congenital TSCS cannot always be prevented, early detection and proactive management can reduce complications:
- Prenatal care and ultrasound can identify spinal anomalies before birth
- Early screening for children with congenital spinal defects
- Prompt evaluation of unexplained lower back pain, leg weakness, or bladder issues
- Careful surgical techniques for spinal procedures to minimize scarring and adhesions
- Awareness of family history and genetic counseling for congenital risk factors
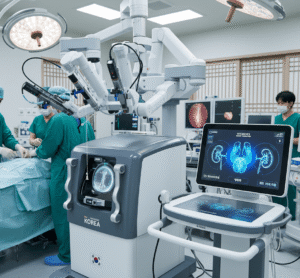
Treatment Options in Korea
Korea provides advanced diagnostic and treatment options for TSCS, focusing on preserving neurological function:
1. Diagnostic Evaluation
- MRI scans: The gold standard for detecting tethered spinal cord and associated abnormalities
- CT scans and X-rays: Used to evaluate spinal bone structures and deformities
- Urodynamic studies: Assess bladder function in affected patients
- Neurological assessments: Evaluate motor and sensory deficits
2. Surgical Treatment
- Detethering surgery: The primary treatment involves surgically releasing the spinal cord from adhesions, lipomas, or other tethering structures.
- Minimally invasive techniques: In selected cases, less invasive approaches reduce tissue damage and recovery time.
- Spinal stabilization procedures: May be combined with detethering in cases with scoliosis or instability.
3. Postoperative Care and Rehabilitation
- Physical therapy to restore mobility, strength, and gait
- Occupational therapy to assist with daily activities
- Bladder and bowel management programs
- Regular follow-up imaging to monitor for re-tethering or recurrence
- Pain management and supportive care as needed
4. Cost and Hospital Care
Treatment costs in Korea vary depending on the complexity of surgery and hospitalization duration. Leading neurosurgical centers provide multidisciplinary care, including preoperative evaluation, state-of-the-art surgical intervention, and comprehensive postoperative rehabilitation. Early intervention ensures optimal neurological recovery and minimizes long-term disability.
With early diagnosis, timely surgery, and structured rehabilitation, patients with TSCS in Korea have excellent prospects for maintaining mobility, bladder control, and overall quality of life.