Overview
Testicular cancer is a malignant growth in one or both testicles, which are part of the male reproductive system responsible for producing sperm and testosterone. Although it is relatively rare compared to other cancers, testicular cancer is the most common cancer in young adult men between ages 15 and 35. South Korea offers advanced diagnostic tools, surgical expertise, and specialized oncology care for testicular cancer, ensuring early detection, effective treatment, and excellent survival rates. Through a combination of medical, surgical, and supportive therapies, Korean healthcare facilities provide comprehensive care tailored to each patient.
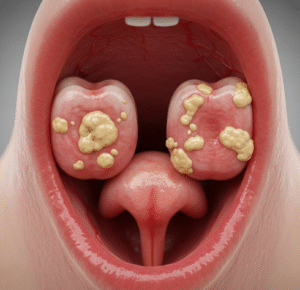
What is Testicular Cancer?
Testicular cancer occurs when abnormal cells in the testicles grow uncontrollably, forming a tumor. These tumors can be classified into two main types:
- Seminomas: Grow slowly and are more sensitive to radiation therapy
- Non-seminomas: Grow more quickly and may consist of several cell types, including embryonal carcinoma, yolk sac tumor, choriocarcinoma, and teratoma
The cancer usually affects only one testicle but can occasionally spread to the other or metastasize to lymph nodes and distant organs. In South Korea, urologists and oncologists work together to diagnose the type, stage, and extent of cancer to determine the most effective treatment approach.
Symptoms
Early symptoms of testicular cancer may be subtle, but recognition is critical for timely treatment:
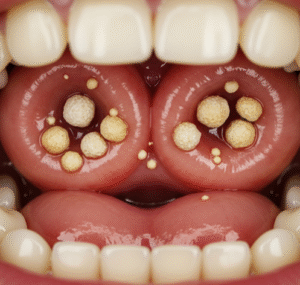
- A painless lump or swelling in one testicle
- A feeling of heaviness or discomfort in the scrotum or lower abdomen
- Pain or discomfort in the testicle or scrotum, occasionally acute
- Enlargement or tenderness of the breasts due to hormonal changes (rare)
- Sudden accumulation of fluid in the scrotum
- Back pain if cancer has spread to lymph nodes
Because early-stage testicular cancer may be asymptomatic, regular self-examination and medical checkups are recommended.
Causes
The exact cause of testicular cancer is not fully understood, but several factors are believed to contribute to its development:
- Undescended testicle (cryptorchidism): Increased risk if one or both testicles fail to descend during fetal development
- Family history: Higher risk if a father or brother had testicular cancer
- Age and gender: Predominantly affects males between 15 and 35
- Previous testicular cancer: Increased risk of developing cancer in the opposite testicle
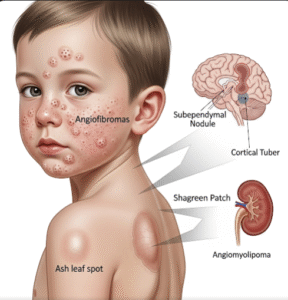
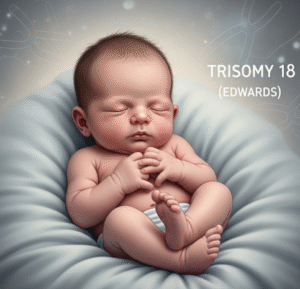
- Genetic conditions: Certain chromosomal abnormalities, such as Klinefelter syndrome
- Environmental factors: Exposure to certain chemicals or radiation may contribute
Korean oncologists evaluate these risk factors to identify high-risk individuals and recommend regular screening.
Risk Factors
Several factors can increase susceptibility to testicular cancer:
- History of cryptorchidism or testicular malformations
- Family history of testicular cancer
- Previous testicular tumors
- Infertility or abnormal testicular development
- Age between 15 and 35, though older men can also be affected
- Race and ethnicity, with higher incidence observed in Caucasian populations
Risk assessment is an integral part of testicular cancer management in South Korea, helping guide early detection and preventive care.
Complications
If left untreated, testicular cancer can lead to serious complications:
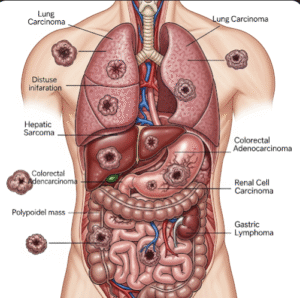
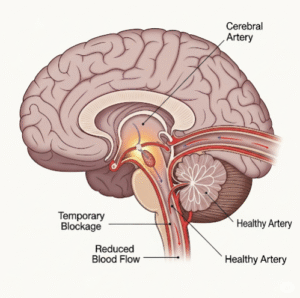
- Spread (metastasis) to lymph nodes, lungs, liver, or brain
- Hormonal imbalances affecting testosterone production
- Infertility due to surgical removal of testicles or chemotherapy effects
- Chronic pain or swelling in the scrotal region
- Side effects from advanced treatments such as chemotherapy or radiotherapy
- Psychological distress related to cancer diagnosis, treatment, or body image changes
Early detection and treatment in Korean hospitals minimize these risks and improve long-term outcomes.
Prevention
While there is no guaranteed way to prevent testicular cancer, several measures may help reduce risk or ensure early detection:
- Regular self-examination: Monthly checks to detect lumps or changes in testicular size
- Awareness of family history: High-risk individuals should undergo regular clinical evaluations
- Prompt medical attention: Seek evaluation for testicular swelling, pain, or other unusual changes
- Healthy lifestyle: Balanced diet, regular exercise, and avoidance of harmful chemicals may support overall reproductive health
- Screening in high-risk groups: Men with cryptorchidism or genetic predispositions should follow physician-recommended screening schedules
Korean healthcare providers emphasize education and awareness campaigns to encourage early detection.
Treatment Options in Korea
Treatment of testicular cancer in South Korea is advanced and tailored to the cancer type, stage, and patient condition:
Diagnosis:
- Physical examination and testicular palpation
- Blood tests for tumor markers such as alpha-fetoprotein (AFP), beta-hCG, and LDH
- Imaging studies including ultrasound, CT scans, and occasionally MRI
- Biopsy or surgical evaluation for definitive diagnosis
Surgical Treatments:
- Orchiectomy: Surgical removal of the affected testicle, often the first-line treatment
- Retroperitoneal lymph node dissection (RPLND): Removal of lymph nodes if cancer has spread
- Testicular prosthesis: Optional placement for cosmetic and psychological reasons
Radiation and Chemotherapy:
- Radiation therapy: Primarily for seminomas, targeting cancer cells while sparing healthy tissue
- Chemotherapy: For advanced or non-seminoma cases, often using combination regimens to ensure effectiveness
Supportive Care and Follow-up:
- Fertility counseling and sperm banking before treatment
- Pain management, psychological support, and nutritional guidance
- Regular follow-up and imaging to monitor recurrence or metastasis
South Korea’s multidisciplinary cancer centers provide a combination of surgical, medical, and supportive care to ensure optimal outcomes, high survival rates, and quality of life for patients with testicular cancer.