Overview
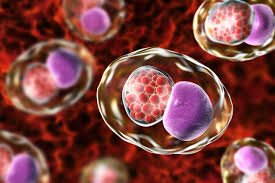
Systemic anthrax is a rare but life-threatening bacterial infection caused by Bacillus anthracis. Unlike localized forms, systemic anthrax spreads throughout the body, affecting multiple organs and often leading to sepsis or meningitis. In Korea, strict biosurveillance and advanced healthcare systems ensure rapid diagnosis and aggressive treatment, making survival possible even in severe cases.
What is Systemic Anthrax?
Systemic anthrax is the disseminated form of anthrax where the Bacillus anthracis bacteria and its toxins spread beyond the initial site of infection into the bloodstream or central nervous system. It can result from untreated cutaneous, inhalational, gastrointestinal, or injection anthrax and often leads to systemic toxemia, septic shock, and multi-organ failure.
Anthrax is classified as a Category A bioterrorism agent due to its potential use in biological warfare. Fortunately, systemic cases are exceedingly rare in Korea due to stringent animal health practices, import controls, and public health policies.
Symptoms
Symptoms vary depending on the route of entry (cutaneous, inhalational, gastrointestinal, or injection), but systemic progression typically includes:
- High fever and chills
- Confusion or altered mental state
- Difficulty breathing
- Rapid heart rate and low blood pressure (signs of septic shock)
- Cyanosis (bluish skin)
- Severe abdominal pain (in GI anthrax)
- Hemorrhagic meningitis (headache, neck stiffness, seizures)
- Multi-organ dysfunction
- Coma (in advanced stages)
Systemic anthrax progresses rapidly and is often fatal without prompt treatment.
Causes
Systemic anthrax is caused by the toxin-producing bacterium Bacillus anthracis. Infection can become systemic if:
- Initial localized infection is not treated promptly
- Spores are inhaled in large amounts
- Immune system fails to contain bacterial growth
- The bacteria release large quantities of anthrax toxins (lethal toxin and edema toxin)
Anthrax spores can survive in soil for decades, and infection is usually contracted through contact with infected animals or contaminated animal products.
Risk Factors
- Occupational exposure (farmers, veterinarians, tannery workers)
- Bioterrorism or laboratory exposure
- Consumption of contaminated meat
- Intravenous drug use (rare, injection anthrax)
- Poor wound care or delayed medical treatment
Although rare in Korea, imported animal products or laboratory exposure may pose potential risks.
Complications
If not treated urgently, systemic anthrax can result in:
- Septic shock
- Hemorrhagic meningitis
- Acute respiratory failure
- Disseminated intravascular coagulation (DIC)
- Multi-organ failure
- Death (mortality can exceed 80% if untreated)
Early recognition and treatment dramatically reduce fatality rates.
Prevention
Korea implements multiple preventive strategies to avoid anthrax outbreaks:
- Livestock vaccination in high-risk zones
- Quarantine regulations on animal imports
- Biosurveillance programs by the Korean Centers for Disease Control and Prevention (KCDC)
- Public awareness campaigns on handling animal products
- Occupational safety protocols for lab workers
- Anthrax vaccine (AVA) available for military personnel and lab workers at risk
Personal prevention includes avoiding undercooked meat from unknown sources and using protective gear in relevant occupations.
Treatment Options in Korea
Korean healthcare facilities are fully equipped to handle rare and emergent infections like systemic anthrax, with state-of-the-art infectious disease units and protocols in place.
Diagnosis
- Blood cultures for Bacillus anthracis
- PCR and ELISA for bacterial DNA or toxins
- Imaging (chest X-ray/CT) to detect inhalational anthrax
- Lumbar puncture if meningitis is suspected
- Laboratory blood tests to evaluate organ function and sepsis
Medications
Treatment is aggressive and often involves:
- IV Antibiotics (Combination therapy):
- Ciprofloxacin or Doxycycline (bactericidal)
- Plus one or more: Clindamycin, Rifampin, or Meropenem
- Antitoxins:
- Raxibacumab or Obiltoxaximab – monoclonal antibodies that neutralize anthrax toxins
- Available under emergency use or strategic national stockpile
- Supportive Intensive Care:
- IV fluids for shock
- Mechanical ventilation if needed
- Vasopressors for hypotension
- Dialysis for kidney failure
- Close monitoring in ICU settings
Post-Exposure Prophylaxis (PEP)
In case of exposure:
- 60-day antibiotic course (ciprofloxacin or doxycycline)
- Anthrax vaccine (3-dose series over 4 weeks)
Korea follows WHO and CDC guidelines for anthrax exposure management.