Overview
Sepsis and septicaemia are serious medical conditions caused by the body’s extreme response to infection. Without prompt treatment, they can lead to tissue damage, organ failure, and death. In Korea, cutting-edge intensive care units (ICUs), rapid diagnostic tools, and standardized treatment protocols have significantly improved outcomes for patients suffering from sepsis.
What is Sepsis and Septicaemia?
- Septicaemia refers to the presence of bacteria in the bloodstream, also known as blood poisoning.
- Sepsis is the body’s overwhelming and life-threatening response to this infection.
Sepsis often progresses from septicaemia and can result in systemic inflammation, reduced blood flow, and organ damage. The two terms are closely related but not exactly the same: septicaemia is an infection in the blood, while sepsis is the broader immune system reaction that can follow.
Symptoms
Common symptoms include:
- High fever or abnormally low body temperature
- Rapid breathing and heart rate
- Confusion or disorientation
- Cold, pale, or mottled skin
- Extreme fatigue or weakness
- Decreased urine output
- Low blood pressure (indicative of septic shock)
These symptoms can develop quickly and require urgent medical attention.
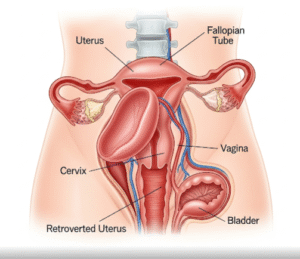
Causes
Sepsis and septicaemia usually develop from:
- Lung infections (e.g., pneumonia)
- Urinary tract infections
- Abdominal infections (e.g., appendicitis, peritonitis)
- Skin infections or infected wounds
- Post-surgical infections
- Infected intravenous lines or catheters
Bacterial infections are the most common cause, but viral and fungal infections can also lead to sepsis.
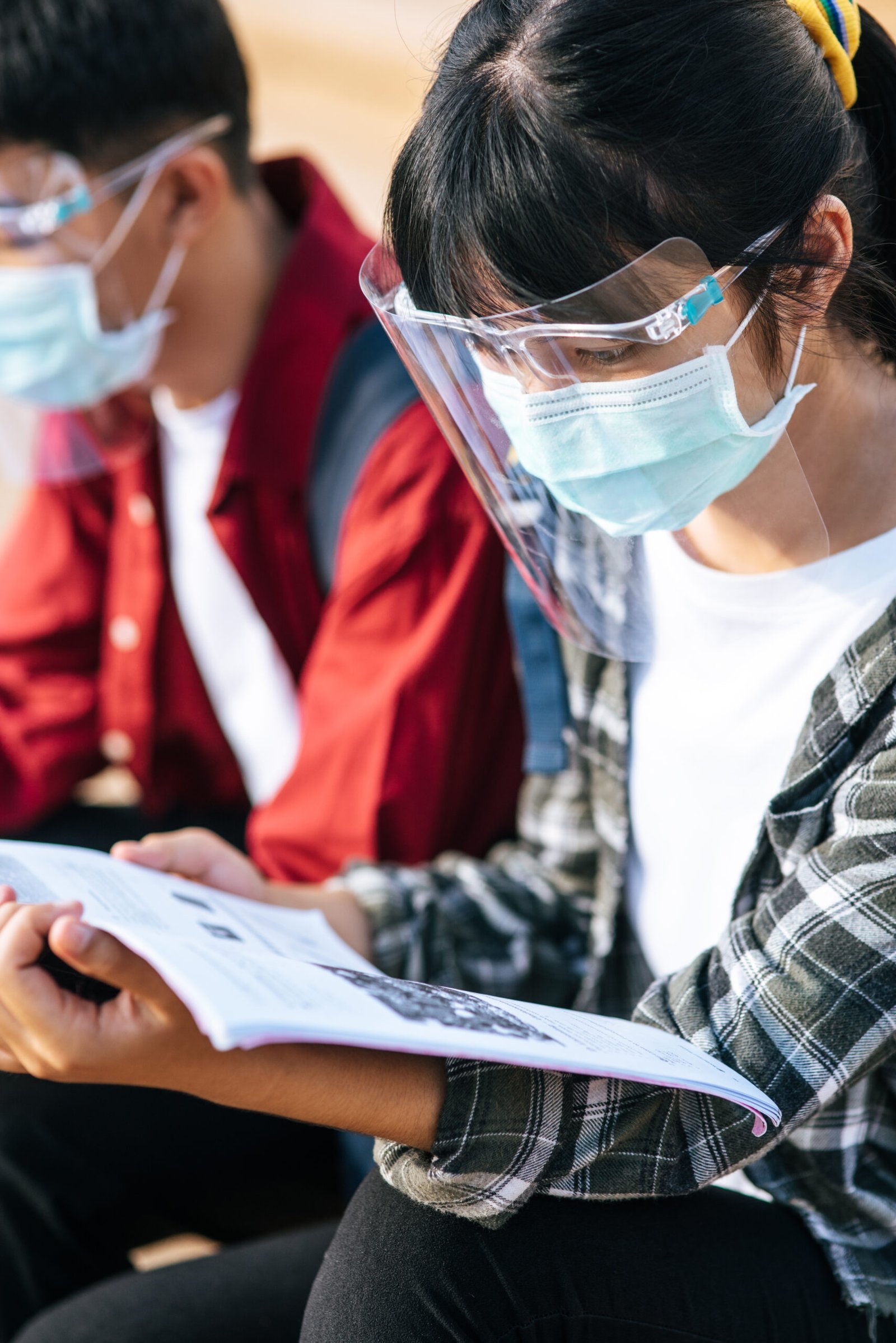
Risk Factors
Individuals at greater risk include:
- Elderly adults and very young children
- People with weakened immune systems (e.g., cancer, HIV)
- Patients with chronic illnesses (e.g., diabetes, kidney disease)
- Recently hospitalized or post-operative patients
- Individuals using invasive medical devices (e.g., catheters, ventilators)
- People with untreated or improperly managed infections
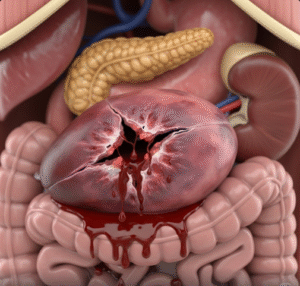
Complications
If not treated promptly, sepsis can result in:
- Septic shock (dangerously low blood pressure)
- Multiple organ failure
- Acute respiratory distress syndrome (ARDS)
- Blood clotting disorders (DIC)
- Death
- Post-sepsis syndrome (long-term fatigue, memory problems, and pain)
Prevention
Prevention strategies include:
- Timely treatment of infections
- Vaccinations (especially for influenza and pneumococcus)
- Proper wound care and hygiene
- Infection control practices in hospitals
- Antibiotic stewardship programs
- Close monitoring of at-risk patients
Treatment Options in Korea
Korea’s hospitals provide globally recognized sepsis care with rapid diagnosis and life-saving interventions.
1. Emergency Diagnosis
- Blood cultures and lab tests (e.g., CRP, lactate)
- Imaging (X-rays, CT scans) to locate infection sources
- Monitoring vital signs and organ function
2. Antibiotic Therapy
- Immediate administration of broad-spectrum IV antibiotics
- Adjustment based on blood culture results
3. Supportive Care
- IV fluids for blood pressure support
- Vasopressors for septic shock
- Oxygen therapy or mechanical ventilation
- Dialysis if kidneys are affected
4. Surgical or Drainage Procedures
- Removal or drainage of infection sources (abscesses, infected tissues)
5. Post-Sepsis Recovery Care
- Physical rehabilitation
- Nutritional and psychological support
- Long-term follow-up