Overview
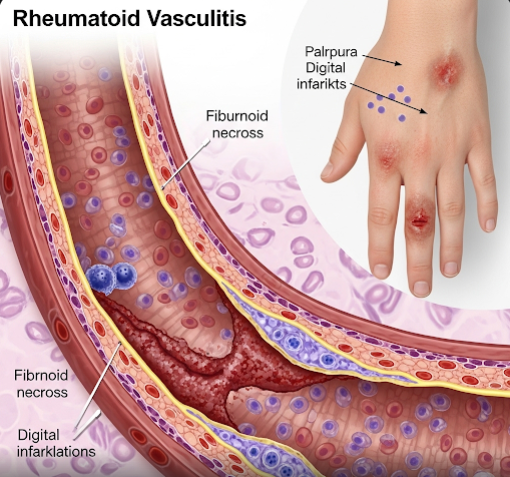
Rheumatoid Vasculitis is a rare but serious complication of rheumatoid arthritis (RA) characterized by inflammation of the blood vessels (vasculitis) due to autoimmune attack. It primarily affects small and medium-sized vessels and can cause tissue damage in various organs. In Korea, early recognition and aggressive treatment in specialized rheumatology centers help manage this condition and reduce associated complications.
What is Rheumatoid Vasculitis?
Rheumatoid Vasculitis occurs when the immune system attacks blood vessel walls in patients with longstanding, severe rheumatoid arthritis. This leads to inflammation and damage of the vessels, impairing blood flow and causing symptoms related to tissue ischemia or organ dysfunction. It is considered a marker of severe RA and often requires intensive therapy.
Symptoms
- Skin ulcers or nodules, especially on the legs and feet
- Pain, numbness, or weakness due to nerve involvement (mononeuritis multiplex)
- Fever and weight loss
- Raynaud’s phenomenon (color changes in fingers/toes)
- Organ-specific symptoms depending on affected vessels (e.g., kidney problems, gastrointestinal pain)
Causes
- Autoimmune inflammation triggered by severe rheumatoid arthritis
- Immune complex deposition in blood vessels causing inflammation
Risk Factors
- Long-standing, severe, or poorly controlled rheumatoid arthritis
- Presence of rheumatoid factor (RF) and anti-CCP antibodies
- Smoking
- Older age
Complications
- Tissue necrosis and ulceration
- Peripheral neuropathy
- Organ damage (kidneys, lungs, gastrointestinal tract)
- Increased risk of infections due to immunosuppressive treatment
Prevention
- Optimal control of rheumatoid arthritis with disease-modifying therapies
- Smoking cessation
- Regular monitoring for early signs of vasculitis in RA patients
Treatment Options in Korea
Korean rheumatology centers provide multidisciplinary care for rheumatoid vasculitis:
- Immunosuppressive Therapy: High-dose corticosteroids and cytotoxic agents (e.g., cyclophosphamide, azathioprine) to control vessel inflammation.
- Biologic Agents: Use of biologics targeting specific immune pathways in refractory cases.
- Symptomatic Management: Wound care for skin ulcers, pain management, and treatment of neuropathy.
- Monitoring: Regular follow-up with blood tests and imaging to assess disease activity and organ function.
- Supportive Care: Physical therapy and rehabilitation for nerve damage.