Overview
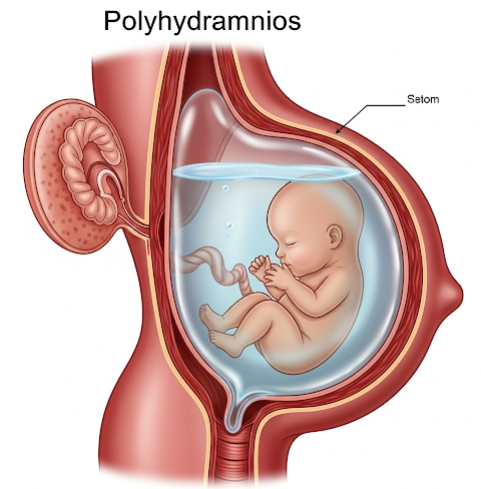
Polyhydramnios is a pregnancy-related condition characterized by an excessive accumulation of amniotic fluid in the uterus. Amniotic fluid is vital for the baby’s growth and development, but when too much fluid builds up, it can lead to complications for both the mother and fetus. While mild cases may resolve on their own, moderate to severe polyhydramnios may require close monitoring or medical intervention. The condition occurs in about 1–2% of pregnancies.
What is Polyhydramnios?
Polyhydramnios is defined when the amniotic fluid index (AFI) exceeds 24 cm, or the deepest vertical pocket (DVP) of fluid measures more than 8 cm on an ultrasound. The condition can be acute (develops quickly) or chronic (develops gradually over time). It can occur in any trimester but is most commonly detected in the second or third trimester.
Symptoms
Many women with mild polyhydramnios have no symptoms. However, moderate to severe cases can cause noticeable discomfort:
- Rapid growth of the uterus
- Abdominal discomfort or tightness
- Difficulty breathing (due to pressure on the diaphragm)
- Swelling in the legs and feet
- Premature uterine contractions
- Decreased fetal movement (in some cases)
- Stretch marks or shiny, tight skin
- Difficulty detecting fetal position or heartbeat on exam
Causes
In many cases, the exact cause of polyhydramnios is unknown (idiopathic). However, it may result from:
- Maternal diabetes (including gestational diabetes)
- Fetal anomalies (e.g., gastrointestinal blockages, neural tube defects)
- Fetal genetic disorders (e.g., trisomy 21, 18, or 13)
- Multiple gestation (twins or more), especially with twin-to-twin transfusion syndrome
- Fetal anemia (e.g., from Rh incompatibility)
- Infections during pregnancy (e.g., cytomegalovirus, toxoplasmosis)
- Placental abnormalities
- Obstructed fetal swallowing or increased fetal urination
Risk Factors
The risk of polyhydramnios may increase due to:
- Poorly controlled diabetes during pregnancy
- Multiple pregnancies (twins, triplets)
- Fetal abnormalities or genetic syndromes
- Infections such as rubella or syphilis
- Maternal age over 35
- History of polyhydramnios in previous pregnancy
- Rh incompatibility
Complications
Polyhydramnios can increase the risk of several maternal and fetal complications:
- Preterm labor and delivery
- Premature rupture of membranes (PROM)
- Placental abruption (detachment from the uterus)
- Umbilical cord prolapse
- Fetal malpresentation (e.g., breech)
- Postpartum hemorrhage
- Cesarean delivery
- Stillbirth (in rare or untreated cases)
Prompt diagnosis and monitoring are essential to reduce the risk of complications.
Prevention
While not all cases can be prevented, you can reduce your risk or manage polyhydramnios more effectively by:
- Controlling blood sugar in diabetic or high-risk pregnancies
- Attending all prenatal checkups for early detection
- Ultrasound screening in mid to late pregnancy
- Testing for infections or fetal abnormalities if needed
- Managing maternal weight and blood pressure
- Avoiding over-the-counter medications without medical approval
Early and regular prenatal care is key to identifying polyhydramnios and minimizing risks.
Treatment Options in Korea
South Korea offers world-class obstetric care, with advanced diagnostic and treatment capabilities for high-risk pregnancies like polyhydramnios.
1. Monitoring and Diagnosis
- Ultrasound measurement of amniotic fluid index (AFI) or DVP
- Fetal anomaly screening via detailed ultrasound and echocardiography
- Glucose tolerance testing for gestational diabetes
- Maternal blood tests for infections or Rh incompatibility
- Non-stress test (NST) and biophysical profile for fetal well-being
2. Medical Management
- Treatment of underlying conditions (e.g., insulin for diabetes)
- Indomethacin therapy (a medication that reduces fetal urine output) – used cautiously
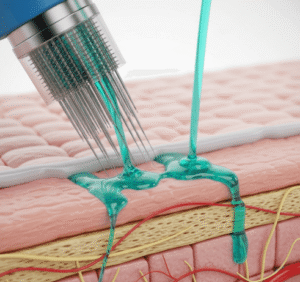
- Amnioreduction: Removing excess amniotic fluid through a needle under ultrasound guidance
- Frequent follow-ups and fetal monitoring
3. Delivery Planning
- Early delivery may be considered if complications arise or if the fluid continues to increase
- Careful planning of timing and method of delivery (vaginal vs. cesarean)
- Immediate availability of neonatal care at delivery
4. Top Hospitals in Korea for Maternity and High-Risk Pregnancy
- Samsung Medical Center
- Seoul National University Hospital
- Asan Medical Center
- Severance Hospital (Yonsei University Health System)
These centers offer:
- Advanced prenatal imaging
- High-risk obstetrics teams
- English-speaking international clinics
- 24/7 neonatal intensive care units (NICU) for preterm or at-risk newborns