Overview
Polyarteritis Nodosa (PAN) is a rare but serious autoimmune disease that causes inflammation of small and medium-sized arteries, leading to organ damage due to reduced blood flow. PAN can affect multiple systems in the body, including the skin, kidneys, heart, gastrointestinal tract, peripheral nerves, and muscles. Without treatment, it can cause severe complications and even become life-threatening. Early diagnosis and immunosuppressive therapy can significantly improve outcomes.
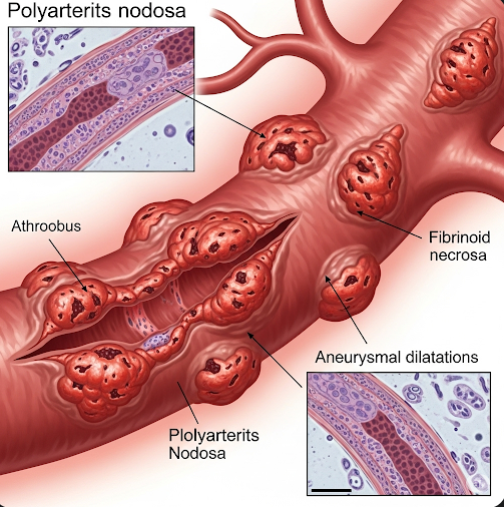
What is Polyarteritis Nodosa?
Polyarteritis Nodosa is a type of systemic vasculitis, meaning it involves widespread inflammation of blood vessels. In PAN, the arteries become swollen and damaged, which may result in aneurysms, clotting, or organ ischemia (lack of blood supply).
It is not associated with ANCA antibodies, which distinguishes it from other forms of vasculitis. While the exact cause is unknown, PAN has been linked to hepatitis B virus infection, and in some cases, other viral or autoimmune triggers.
Symptoms
Symptoms of PAN can vary depending on which organs are affected. The condition typically presents gradually, but it may also begin suddenly and severely.
General Symptoms:
- Fever
- Fatigue and weakness
- Weight loss
- Night sweats
- Muscle and joint aches
Organ-Specific Symptoms:
- Skin: Livedo reticularis (mottled rash), painful nodules, ulcers
- Nerves: Numbness, tingling, weakness, foot or wrist drop
- Kidneys: High blood pressure, kidney dysfunction
- Gastrointestinal tract: Abdominal pain (especially after eating), nausea, vomiting, bowel perforation in severe cases
- Heart: Chest pain, heart attack, heart failure
- Testicles: Pain or tenderness (orchitis)
Without treatment, PAN can progress and cause serious multi-organ failure.
Causes
The exact cause of PAN is unknown in most cases, but several triggers or associations have been identified:
- Hepatitis B virus (HBV) – historically a major cause, though now less common with vaccination
- Hepatitis C virus (HCV) – rarely associated
- Immune system dysfunction – possibly autoimmune in nature
- Genetic predisposition – especially in familial PAN or in children
- Certain medications or infections – may rarely trigger PAN
PAN is not contagious, and most cases are considered idiopathic (of unknown origin).
Risk Factors
Factors that may increase the risk of PAN include:
- Hepatitis B infection
- Male gender (PAN is more common in men than women)
- Age between 40–60 years
- Autoimmune diseases or immune dysregulation
- Family history of vasculitis (rare hereditary forms)
- Certain viral infections
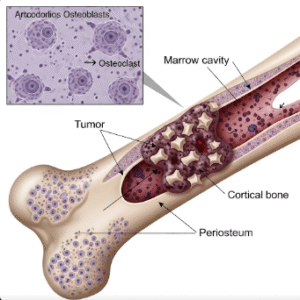
Complications
If not treated early, PAN can cause severe and sometimes fatal complications:
- Kidney failure
- Stroke or heart attack
- Bowel infarction or perforation
- Peripheral neuropathy (nerve damage)
- Skin necrosis or gangrene
- High blood pressure that is difficult to control
- Organ damage or failure (e.g., heart, liver, lungs)
- Death, especially in untreated or severe cases
Prevention
There is no known way to completely prevent PAN, but the risk may be reduced by:
- Vaccination against hepatitis B
- Avoiding hepatitis B and C exposure (safe practices, clean needles, protected sex)
- Regular health checkups if at high risk
- Prompt treatment of underlying infections
- Avoiding unregulated medications or toxins
For patients with PAN, early diagnosis and adherence to treatment are key to preventing complications.
Treatment Options in Korea
South Korea offers world-class care for rare autoimmune diseases like PAN, with comprehensive support from rheumatology, nephrology, neurology, and internal medicine departments.
1. Medications
- Corticosteroids (e.g., prednisone): First-line treatment to reduce inflammation
- Immunosuppressants:
- Cyclophosphamide for severe or organ-threatening disease
- Azathioprine or methotrexate for maintenance therapy
- Antiviral therapy if PAN is related to hepatitis B infection
- Antihypertensives to manage high blood pressure
- Pain relievers for nerve and joint pain
2. Monitoring and Supportive Care
- Regular blood tests and imaging to monitor organ function and treatment response
- Renal function monitoring
- Neurological assessments for nerve damage
- Wound care for skin ulcers or lesions
3. Hospitalization (for Severe Cases)
- Required for patients with organ failure, severe hypertension, or life-threatening complications
4. Long-Term Management
- Gradual tapering of immunosuppressants once stable
- Physical therapy for muscle weakness or neuropathy
- Psychological support for coping with chronic illness
5. Top Hospitals in Korea
Major Korean medical centers like Asan Medical Center, Samsung Medical Center, Severance Hospital, and Seoul National University Hospital provide:
- Specialized rheumatology clinics for systemic vasculitis
- Multidisciplinary teams to handle organ-specific complications
- English-speaking specialists and international care coordination
- Access to clinical trials and advanced biologic therapies (in select cases)