Overview
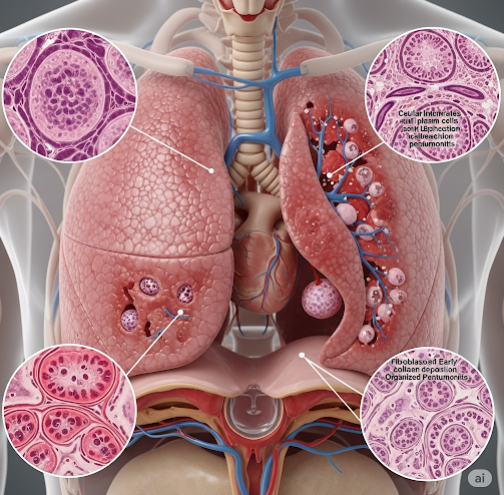
Pneumonitis refers to inflammation of the lung tissue, specifically the alveoli (air sacs), often caused by an allergic reaction, infection, or exposure to irritants such as chemicals, radiation, or certain medications. Unlike pneumonia, which is typically caused by infection, pneumonitis is usually non-infectious in origin. If not properly diagnosed and treated, pneumonitis can progress to chronic lung damage and pulmonary fibrosis. Early recognition is key to preventing irreversible complications.
What is Pneumonitis?
Pneumonitis is an inflammatory condition of the lung parenchyma that causes the alveoli to fill with fluid or cellular debris, leading to impaired oxygen exchange. The term encompasses a wide range of non-infectious inflammatory lung disorders, and its presentation varies depending on the cause and extent of inflammation.
Types of pneumonitis include:
- Hypersensitivity pneumonitis (extrinsic allergic alveolitis) – immune response to inhaled allergens
- Radiation pneumonitis – from radiation therapy to the chest
- Drug-induced pneumonitis – side effect of medications
- Chemical pneumonitis – inhalation of toxic substances like chlorine gas or smoke
- Autoimmune pneumonitis – associated with systemic conditions like lupus or rheumatoid arthritis
Symptoms
Pneumonitis may present acutely, subacutely, or chronically, depending on the cause and exposure.
Common symptoms include:
- Dry, nonproductive cough
- Shortness of breath, especially with exertion
- Fatigue or malaise
- Chest discomfort or tightness
- Fever (occasionally)
- Weight loss and muscle aches (in chronic cases)
- Crackles heard on lung auscultation
Symptoms of chronic pneumonitis may mimic other lung diseases like asthma or pulmonary fibrosis.
Causes
Pneumonitis can be triggered by a wide variety of agents, broadly categorized as:
- Environmental or Occupational Exposure
- Mold, bird droppings, hay, and dust (hypersensitivity pneumonitis)
- Agricultural work, hot tubs, humidifiers, or metalworking fluids
- Radiation Therapy
- Especially in patients receiving radiation for breast, lung, or lymphoma cancers
- Often appears 1–6 months after radiation exposure
- Medications
- Chemotherapy drugs (e.g., methotrexate, bleomycin)
- Immunotherapy agents (e.g., checkpoint inhibitors)
- Antibiotics like nitrofurantoin
- Autoimmune Disorders
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Sjögren’s syndrome
- Inhaled Toxins or Fumes
- Smoke inhalation
- Chlorine or ammonia exposure
- Aspiration of gastric contents (chemical pneumonitis)
Risk Factors
The likelihood of developing pneumonitis increases with:
- Exposure to organic or chemical dusts
- Receiving radiation therapy, especially to the chest
- Use of pneumonitis-associated medications
- Working in agriculture, metalwork, or bird handling
- Autoimmune diseases
- Immunocompromised status
- Older age, due to reduced lung reserve
Complications
If not diagnosed and treated in time, pneumonitis can lead to:
- Chronic inflammation and scarring of lung tissue (pulmonary fibrosis)
- Respiratory failure
- Persistent shortness of breath or cough
- Reduced quality of life and exercise capacity
- Misdiagnosis as asthma, COPD, or infection, leading to inappropriate treatment
- Death, in severe untreated or progressive cases
Prevention
While not all types of pneumonitis are preventable, the following steps can help reduce risk:
- Avoid known environmental triggers (dust, mold, chemicals)
- Use protective gear in high-risk workplaces
- Inform your doctor about all medications and prior radiation treatments
- Avoid smoking, which worsens lung inflammation
- Regular follow-ups if you are on immunotherapy or chemotherapy
- Promptly report respiratory symptoms if you have autoimmune conditions or recent exposure to triggers
Treatment Options in Korea
South Korea offers advanced diagnostic tools and multidisciplinary treatment for pneumonitis through its leading pulmonology and internal medicine departments.
1. Diagnosis
- High-resolution chest CT (HRCT): reveals ground-glass opacities or fibrosis
- Pulmonary function tests (PFTs): to assess lung capacity and gas exchange
- Bronchoscopy with lavage: to rule out infection or malignancy
- Blood tests: to identify autoimmune markers or eosinophils
- Lung biopsy: in complex or unresolved cases
2. Treatment Based on Cause
- Corticosteroids (e.g., prednisone): Mainstay of treatment for most types of pneumonitis
- Immunosuppressants (azathioprine, methotrexate): For autoimmune-related pneumonitis
- Discontinuation of the causative drug or exposure
- Oxygen therapy: For patients with hypoxia
- Bronchodilators: To ease breathing in some cases
- Antibiotics: Only if there is evidence of secondary infection
- Antifibrotic drugs: For patients progressing to pulmonary fibrosis
3. Long-Term Management
- Regular lung function monitoring
- Pulmonary rehabilitation for chronic symptoms
- Vaccination (flu, pneumococcal) to prevent secondary infections
- Lifestyle adjustments to limit exposure to triggers
- Patient education and respiratory health coaching
4. Leading Hospitals in Korea
Top-tier institutions like Samsung Medical Center, Asan Medical Center, Severance Hospital, and Seoul National University Hospital provide:
- Expert pulmonologists and interstitial lung disease specialists
- Advanced imaging and minimally invasive diagnostics
- English-speaking services for international patients
- Coordinated care for cancer patients, autoimmune disorders, and occupational lung disease