Overview
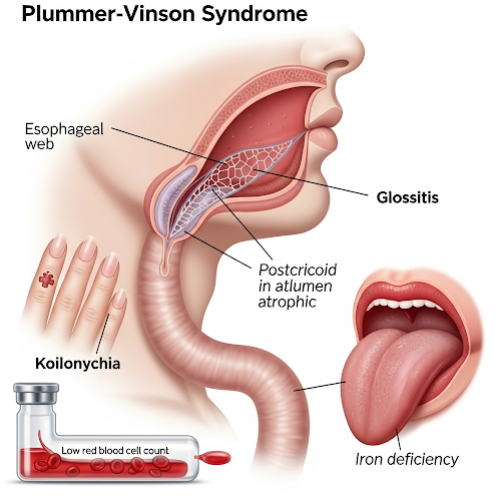
Plummer-Vinson Syndrome (PVS) is a rare condition characterized by the triad of iron-deficiency anemia, difficulty swallowing (dysphagia), and esophageal webs — thin membranes that partially block the upper esophagus. It primarily affects middle-aged women, especially those of Northern European descent, but cases have been reported worldwide. While the syndrome itself is treatable, it is considered precancerous and may increase the risk of developing esophageal or pharyngeal cancer if left unmanaged.
What is Plummer-Vinson Syndrome?
Plummer-Vinson Syndrome (also known as Paterson-Brown-Kelly syndrome) involves iron deficiency that leads to mucosal and muscular atrophy, particularly in the upper esophagus. This causes the formation of esophageal webs, which are thin membranes that narrow the esophageal lumen and interfere with swallowing.
Although the exact mechanism isn’t fully understood, iron deficiency appears to impair epithelial cell repair and muscle function, contributing to the syndrome’s symptoms.
Symptoms
The hallmark symptoms of PVS include:
- Difficulty swallowing (dysphagia) — typically for solids, due to esophageal narrowing
- Fatigue and weakness — resulting from iron-deficiency anemia
- Glossitis — smooth, inflamed tongue
- Angular cheilitis — cracks or sores at the corners of the mouth
- Pale skin or mucous membranes
- Brittle nails or spoon-shaped nails (koilonychia)
- Shortness of breath on exertion
- Weight loss (if dysphagia is prolonged)
Symptoms may develop gradually and are often subtle until anemia becomes more severe.
Causes
The primary cause of Plummer-Vinson Syndrome is iron deficiency, which may result from:
- Poor dietary intake of iron
- Chronic blood loss (e.g., heavy menstrual bleeding, gastrointestinal bleeding)
- Malabsorption syndromes (e.g., celiac disease)
- Increased iron requirement (e.g., during pregnancy)
- Autoimmune conditions (suggested in some cases)
While iron deficiency is the key factor, genetic and environmental components may also contribute to the formation of esophageal webs.
Risk Factors
Several factors increase the risk of developing Plummer-Vinson Syndrome:
- Gender: More common in females
- Age: Typically seen in adults between 40–70 years old
- Nutritional deficiencies: Especially iron and B vitamins
- Chronic blood loss: Menorrhagia or gastrointestinal bleeding
- Low socioeconomic status or malnutrition
- Geographic origin: Historically more common in Northern Europe, though now rare due to improved nutrition
- Family history of anemia or esophageal disorders
Complications
If untreated, Plummer-Vinson Syndrome can lead to:
- Esophageal stricture — persistent narrowing of the esophagus
- Malnutrition — due to poor oral intake
- Aspiration — food entering the airway during swallowing
- Increased risk of squamous cell carcinoma of the esophagus, pharynx, or oral cavity
- Recurrent anemia or fatigue
- Chronic swallowing difficulties impacting quality of life
Prevention
There is no guaranteed way to prevent PVS, but addressing iron deficiency and maintaining good nutritional health can greatly reduce the risk. Preventive strategies include:
- Consuming iron-rich foods: such as red meat, beans, dark leafy greens, and fortified cereals
- Taking iron supplements when medically indicated
- Monitoring iron levels during high-risk periods (e.g., pregnancy or heavy menstruation)
- Early treatment of chronic blood loss or gastrointestinal issues
- Routine medical check-ups to detect anemia early
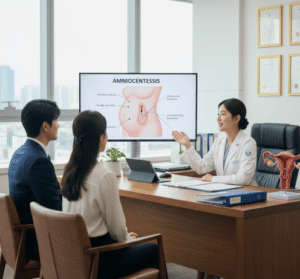
Treatment Options in Korea
South Korea offers advanced gastroenterological and nutritional care, making it an excellent destination for diagnosing and managing Plummer-Vinson Syndrome. Treatment generally involves a multimodal approach:
1. Iron Supplementation
- Oral iron therapy (ferrous sulfate or ferrous gluconate) to correct iron deficiency
- Intravenous iron in cases of poor absorption or severe anemia
- Treatment typically improves symptoms and may reduce or eliminate esophageal webs
2. Nutritional Support
- Dietary counseling with a nutritionist
- Vitamin supplementation (especially B12 and folate if deficient)
- Management of underlying causes of malabsorption or chronic blood loss
3. Esophageal Dilation
- Endoscopic dilation procedures used to widen the esophagus and relieve dysphagia
- Often performed in outpatient settings under sedation
- Repeat dilations may be necessary for recurring webs
4. Monitoring for Cancer
- Regular upper endoscopy (EGD) to monitor for malignant changes
- Biopsy of suspicious lesions during endoscopy
- Oncology referral if cancer is detected early
5. Long-Term Follow-Up
- Regular monitoring of iron levels and blood counts
- Ongoing nutritional assessment
- Speech and swallowing therapy for patients with persistent dysphagia
6. International Care Services
Leading Korean hospitals such as Seoul National University Hospital, Asan Medical Center, Samsung Medical Center, and Severance Hospital offer:
- Multidisciplinary care involving gastroenterology, ENT, and hematology
- English-speaking providers and interpreters
- Advanced diagnostic tools (endoscopy, imaging, labs)
- Customized treatment plans for international patients