Overview
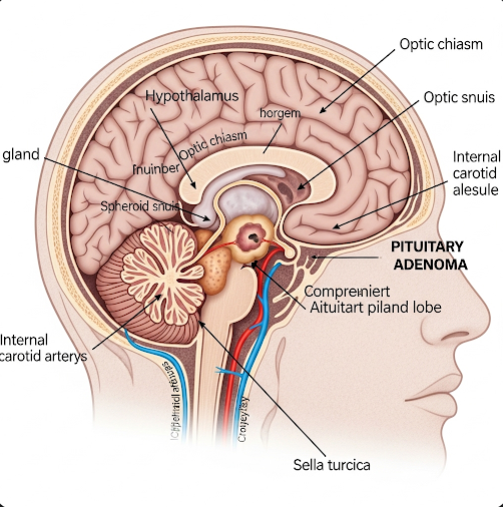
Pituitary adenoma is a generally benign (non-cancerous) tumor that develops in the pituitary gland, a small but vital endocrine gland located at the base of the brain. Although most pituitary adenomas are slow-growing and noncancerous, they can affect hormone production and compress nearby brain structures, leading to a wide range of hormonal, neurological, and visual symptoms. With early diagnosis and appropriate treatment, most pituitary adenomas can be managed effectively.
What is Pituitary Adenoma?
A pituitary adenoma is a growth or tumor originating in the anterior pituitary gland, which is responsible for producing essential hormones that regulate growth, reproduction, metabolism, and stress response. These tumors are categorized as:
- Functioning (hormone-producing) adenomas – secrete excess hormones
- Non-functioning (non-secreting) adenomas – do not produce hormones but may cause symptoms due to size or pressure
Functioning adenomas are further classified based on the hormone they secrete:
- Prolactinomas – produce excess prolactin
- Growth hormone (GH)-secreting tumors – cause acromegaly or gigantism
- Adrenocorticotropic hormone (ACTH)-secreting tumors – lead to Cushing’s disease
- Thyroid-stimulating hormone (TSH)-secreting tumors – rare, may cause hyperthyroidism
Symptoms
Symptoms vary depending on whether the tumor is functioning or non-functioning, and its size. Common symptoms include:
Hormonal Symptoms (due to excess hormone production):
- Irregular menstruation or infertility (prolactinoma)
- Enlarged hands, feet, or facial features (acromegaly)
- Weight gain, high blood pressure, and round face (Cushing’s disease)
- Heat intolerance, palpitations (hyperthyroidism from TSH tumors)
Mass Effect Symptoms (due to tumor size):
- Persistent headaches
- Vision problems (especially loss of peripheral vision)
- Fatigue or weakness
- Nausea and vomiting
- Decreased libido or erectile dysfunction
- Symptoms of hypopituitarism (if normal hormone production is suppressed)
Causes
The exact cause of pituitary adenomas is not fully understood, but contributing factors may include:
- Genetic mutations affecting pituitary cell growth and regulation
- Familial syndromes such as Multiple Endocrine Neoplasia type 1 (MEN1)
- Spontaneous cell changes in the pituitary gland
- Environmental triggers are suspected in rare cases, but not proven
Most pituitary adenomas occur sporadically and are not inherited.
Risk Factors
While pituitary adenomas can affect anyone, certain factors may increase the risk:
- Age (most common between 30–50 years old)
- Family history of pituitary tumors or MEN1 syndrome
- Female gender (especially for prolactinomas)
- Genetic disorders (e.g., Carney complex, McCune-Albright syndrome)
- Exposure to radiation (rare)
Complications
If left untreated, pituitary adenomas can lead to serious complications:
- Vision loss due to compression of the optic chiasm
- Permanent hormonal imbalances (hypopituitarism)
- Osteoporosis, infertility, or sexual dysfunction
- Acromegaly-related complications (heart disease, joint issues)
- Cushing’s disease complications (diabetes, high blood pressure)
- Pituitary apoplexy – sudden bleeding into the tumor, a medical emergency causing severe headache and loss of consciousness
Prevention
There is no definitive way to prevent pituitary adenomas. However, early detection and treatment can reduce complications. Preventive strategies include:
- Regular checkups for individuals with a family history of endocrine tumors
- Monitoring for hormone-related symptoms such as irregular periods, unusual growth, or visual changes
- Genetic counseling for families with hereditary endocrine disorders
- Prompt evaluation of persistent headaches and vision problems
Treatment Options in Korea
South Korea offers world-class care for pituitary adenomas through a combination of advanced neurosurgery, endocrinology, and medical imaging. Treatment depends on tumor size, type, and hormone activity:
1. Medication
- Dopamine agonists (e.g., cabergoline, bromocriptine) – for prolactinomas
- Somatostatin analogs (e.g., octreotide) or GH receptor blockers – for acromegaly
- Adrenal inhibitors – to manage Cushing’s disease before surgery
- Thyroid control medications – for TSH-secreting tumors
2. Surgery
- Transsphenoidal surgery: Minimally invasive procedure performed through the nose to remove the tumor
- Endoscopic techniques are widely used in Korea, allowing precise removal with minimal complications
- Craniotomy: Required for very large or inaccessible tumors
3. Radiation Therapy
- Stereotactic radiosurgery (e.g., Gamma Knife) – highly focused radiation for tumors that cannot be fully removed surgically
- Conventional radiation therapy – used for recurring or residual tumors
4. Hormone Replacement Therapy
- For patients who develop hypopituitarism (underproduction of hormones), lifelong hormone replacement (e.g., cortisol, thyroid hormone, sex hormones, GH) may be required
5. Diagnostic Support in Korea
- MRI with contrast – high-resolution brain imaging to evaluate tumor size and impact
- Endocrine testing – blood tests to assess hormone levels
- Ophthalmologic exams – to assess vision loss from optic nerve compression
6. International Care Services
Leading hospitals such as Severance Hospital, Samsung Medical Center, and Seoul National University Hospital offer:
- Multidisciplinary pituitary tumor centers
- English-speaking endocrinologists and neurosurgeons
- Integrated care with surgery, hormone therapy, and follow-up services
- Personalized care for international patients, including medical visas and translation support
South Korea’s advanced diagnostics, highly skilled neurosurgical teams, and modern endocrine therapies make it one of the best places to receive effective treatment for pituitary adenomas.