Overview
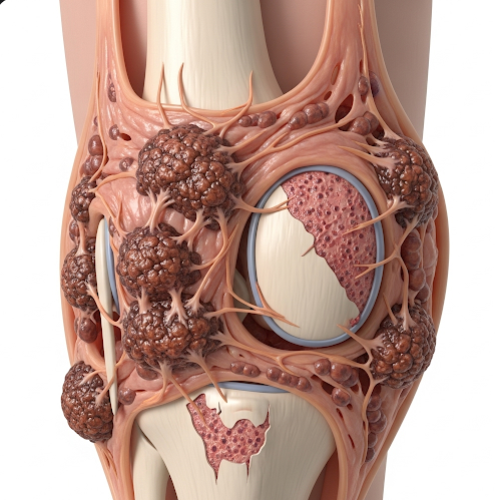
Pigmented Villonodular Synovitis (PVNS) is a rare, benign but locally aggressive joint condition that causes abnormal thickening and overgrowth of the synovium — the soft tissue lining the joints and tendons. It typically affects a single joint, most commonly the knee, followed by the hip, ankle, and shoulder. Though non-cancerous, PVNS can lead to joint damage, pain, swelling, and reduced mobility over time if not treated appropriately.
What is Pigmented Villonodular Synovitis?
PVNS is characterized by an abnormal proliferation of the synovial membrane accompanied by the deposition of hemosiderin (a pigment from blood breakdown), giving the condition its “pigmented” name. The overgrown synovium may form nodules or villi (finger-like projections), leading to mechanical wear and inflammation in the joint.
There are two main types:
- Localized PVNS – confined to a specific area of the synovium, often forming a nodule
- Diffuse PVNS – affects a larger portion or the entire synovial membrane, typically more aggressive and recurrent
PVNS most commonly affects adults aged 20–50 and occurs equally in men and women.
Symptoms
Symptoms of PVNS can develop gradually and may mimic more common joint disorders like arthritis. Common signs include:
- Persistent joint swelling
- Joint pain or aching, often worsening with activity
- Stiffness and reduced range of motion
- Joint instability or locking
- Warmth around the joint
- Joint effusion (fluid buildup)
- Muscle atrophy in chronic cases
In some patients, symptoms may fluctuate or be misdiagnosed for years before a correct diagnosis is made.
Causes
The exact cause of PVNS is still unclear. Several theories suggest:
- Inflammatory response: Chronic irritation of the synovium may lead to abnormal growth
- Trauma-related triggers: Previous joint injury may stimulate excessive synovial proliferation
- Genetic mutations: Recent research suggests a possible neoplastic (tumor-like) origin involving chromosomal abnormalities
- Spontaneous development: Many cases occur without any identifiable risk factor
Though non-cancerous, PVNS behaves in a tumor-like manner and can invade nearby tissues.
Risk Factors
While PVNS is rare, certain factors may increase the likelihood of developing the condition:
- Age: Most commonly affects people between 20 and 50 years old
- Joint trauma: A history of joint injury or surgery
- Joint overuse: Repetitive movement or mechanical stress
- Previous inflammatory joint disease
- No gender bias, but diffuse PVNS may be slightly more common in men
Complications
If left untreated or improperly managed, PVNS can lead to serious joint problems, including:
- Cartilage damage and joint destruction
- Recurrent joint effusion
- Chronic pain and stiffness
- Joint deformity and disability
- Osteoarthritis secondary to PVNS
- Recurrence after surgery, especially in diffuse cases
- Reduced mobility and quality of life
In very rare cases, PVNS may affect bones or extend beyond the joint, though it remains non-metastatic.
Prevention
There is currently no known way to prevent PVNS, but early detection and proper treatment are essential for preventing joint damage. Preventive strategies are limited but may include:
- Prompt evaluation of unexplained joint swelling or pain
- Regular follow-up after joint trauma or surgery
- Imaging studies for persistent or recurrent joint issues
- Avoiding prolonged neglect of joint symptoms
- Maintaining joint health through proper physical therapy if at risk
Treatment Options in Korea
South Korea offers cutting-edge diagnostic imaging and multidisciplinary orthopedic care, making it a leading destination for the treatment of Pigmented Villonodular Synovitis. Available treatments include:
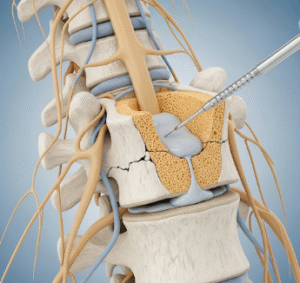
- Arthroscopic synovectomy: A minimally invasive surgery to remove the overgrown synovial tissue. Commonly used for localized PVNS, especially in the knee or ankle
- Open synovectomy: Required in more extensive (diffuse) cases or in larger joints like the hip
- Radiotherapy or radiosynoviorthesis: In cases of recurrent PVNS or when surgery isn’t feasible, radioactive treatment can help control synovial proliferation
- Targeted drug therapy: Newer treatments like CSF1R inhibitors (colony-stimulating factor 1 receptor blockers) are available in clinical trials or specialized centers for advanced or inoperable PVNS
- Advanced imaging diagnostics: High-resolution MRI is essential for diagnosis, monitoring recurrence, and planning surgery
- Rehabilitation therapy: Post-surgical physiotherapy to restore joint function and mobility
- Long-term follow-up: Korean orthopedic centers provide structured monitoring for early detection of recurrence
- International patient care: Top hospitals such as Seoul National University Hospital, Asan Medical Center, and Severance Hospital offer English-language services and comprehensive orthopedic programs for international patients
With its advanced orthopedic and rheumatology departments, Korea provides effective, patient-centered care for even rare joint disorders like PVNS, combining surgical expertise with the latest treatment innovations.