Overview
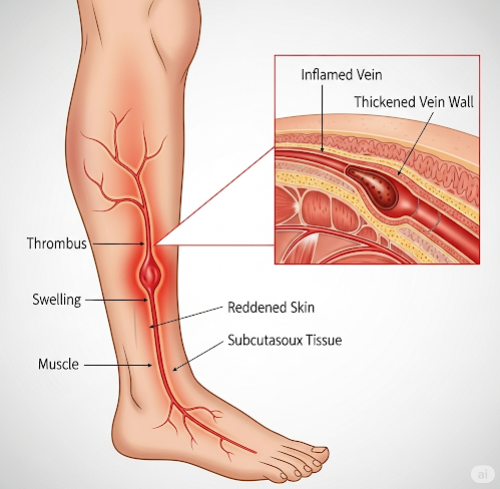
Phlebitis is the inflammation of a vein, usually occurring in the legs. It may affect superficial veins (superficial phlebitis) or deeper veins (deep vein thrombophlebitis or DVT). While superficial phlebitis is often mild and self-limiting, DVT can be more serious and may lead to life-threatening complications such as pulmonary embolism. Early diagnosis and treatment are important to prevent progression and reduce the risk of complications.
What is Phlebitis?
Phlebitis refers to the inflammation of a vein, which may be caused by infection, injury, or irritation. It often manifests as redness, swelling, and pain along the vein. When the inflamed vein develops a blood clot, the condition is known as thrombophlebitis. The condition is more common in people who are immobile for extended periods or have underlying vascular or clotting disorders.
Symptoms
Common signs and symptoms of phlebitis include:
- Redness and warmth along the affected vein
- Swelling of the surrounding skin or tissue
- Pain or tenderness at the site
- Hardening or thickening of the vein (like a cord under the skin)
- Low-grade fever in some cases
- If deep veins are involved, there may be leg swelling, heaviness, and discomfort
Causes
Phlebitis can be triggered by several factors, including:
- Prolonged immobility or bed rest
- Intravenous catheters or IV medications that irritate the veins
- Varicose veins
- Trauma or injury to a vein
- Infections
- Autoimmune conditions
- Blood clotting disorders
- Use of birth control pills or hormone replacement therapy
Risk Factors
Factors that may increase the risk of phlebitis include:
- Recent surgery or hospitalization
- Smoking
- Obesity
- Pregnancy or postpartum state
- Advanced age
- Family history of clotting disorders
- Cancer or undergoing chemotherapy
- Long periods of travel without movement (e.g., flights, car rides)
Complications
If left untreated, phlebitis—especially deep vein thrombophlebitis—can lead to serious health issues such as:
- Pulmonary embolism (a life-threatening condition caused by a blood clot traveling to the lungs)
- Post-thrombotic syndrome (chronic pain and swelling in the leg)
- Chronic venous insufficiency
- Recurrent thrombophlebitis
- Skin ulcers around the affected area
Prevention
Several measures can help prevent phlebitis, especially in high-risk individuals:
- Stay active and avoid prolonged periods of immobility
- Stretch or walk during long flights or car rides
- Use compression stockings if prescribed
- Maintain a healthy weight
- Stay hydrated
- Avoid smoking
- Follow your doctor’s guidance after surgery to prevent blood clots
- Ensure IV lines are properly managed in hospital settings
Treatment Options in Korea
South Korea is known for its highly advanced vascular care and minimally invasive procedures. Treatments for phlebitis available in Korean hospitals include:
- Anti-inflammatory medications: Such as NSAIDs to reduce pain and swelling
- Anticoagulant therapy: For cases involving blood clots, doctors may prescribe blood thinners (e.g., heparin, warfarin, or DOACs)
- Compression therapy: Medical-grade compression stockings improve blood flow and reduce swelling
- IV catheter management: Removal or replacement of any irritating IV lines
- Laser or radiofrequency ablation: For patients with varicose veins causing recurrent phlebitis, Korean clinics offer advanced vein ablation treatments
- Ultrasound-guided care: High-resolution imaging is used for precise diagnosis and to monitor deep vein health
- Specialized vascular clinics: Many large hospitals in Seoul and other cities have departments focused exclusively on vein health and thrombosis care, with English-speaking staff and streamlined care for international patients