Overview
Phantom Limb Syndrome (PLS) is a condition in which individuals experience sensations—including pain—in a limb that has been amputated. Although the limb is physically absent, the brain continues to perceive its presence. These sensations can be mild or severe and may persist for months or years after amputation. Phantom limb pain is common and can interfere with daily life, emotional well-being, and rehabilitation if not properly managed.
What is Phantom Limb Syndrome?
Phantom Limb Syndrome occurs after the surgical removal or traumatic loss of a body part, most often a leg or arm. Despite the limb being gone, patients may continue to feel pain, itching, pressure, or even movement in the missing part. These sensations are believed to originate from the brain and spinal cord, not the site of amputation itself.
PLS includes two categories:
- Phantom Sensations: Non-painful feelings like tingling, pressure, or movement.
- Phantom Limb Pain (PLP): Painful sensations perceived in the absent limb—ranging from stabbing and burning to cramping or throbbing.
Symptoms
Symptoms of Phantom Limb Syndrome may vary widely in frequency, intensity, and duration:
- Burning, stabbing, shooting, or throbbing pain in the missing limb
- Tingling or pins-and-needles sensations
- Sensations of movement or cramping in the absent limb
- Feeling of the limb being in an awkward or painful position
- Sensation that the limb is still present or attached
- Intermittent or constant episodes of discomfort
Symptoms often begin within a few days of amputation but can also appear weeks or months later.
Causes
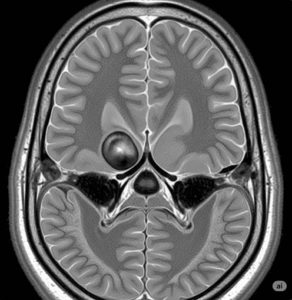
The exact cause of Phantom Limb Syndrome is not fully understood, but several theories explain its occurrence:
- Neurological reorganization: After amputation, the brain and spinal cord reorganize how they process sensory input, which can result in abnormal signals being interpreted as pain or sensation.
- Peripheral nerve damage: Nerve endings at the amputation site may send faulty signals to the brain.
- Psychological components: Emotional trauma, grief, and stress may exacerbate the perception of phantom pain.
- Brain map confusion: The brain’s sensory map still includes the missing limb, creating the illusion of its presence.
Risk Factors
Several factors can increase the likelihood of developing Phantom Limb Syndrome:
- Amputation due to traumatic injury
- Presence of chronic pain before the amputation
- Poor post-surgical pain management
- Emotional distress or post-traumatic stress disorder (PTSD)
- Lack of prosthetic use or rehabilitation
- Nerve-related conditions (e.g., neuromas)
While PLS can affect people of any age, it is more common among adults who have lost major limbs.
Complications
Phantom Limb Syndrome can lead to significant complications if left untreated:
- Chronic pain and discomfort
- Sleep disturbances
- Depression and anxiety
- Reduced quality of life
- Difficulty using prosthetic limbs
- Social withdrawal or emotional distress
It may also interfere with physical rehabilitation, making it harder for patients to regain independence.
Prevention
Although not always preventable, certain strategies can help reduce the risk or severity of PLS:
- Effective pain control before and after amputation (e.g., nerve blocks, epidurals)
- Early use of a prosthetic limb to help the brain adjust to the loss
- Pre-amputation counseling and psychological support
- Mirror therapy or visual feedback immediately after surgery
- Proper surgical techniques that minimize nerve damage
These preventive steps are especially important for patients undergoing planned (non-emergency) amputations.
Treatment Options in Korea
South Korea offers advanced multidisciplinary approaches to manage Phantom Limb Syndrome through a combination of pain management, physical therapy, and cutting-edge technology.
- Pharmacological Treatments:
- Pain relievers such as NSAIDs or opioids (for short-term use)
- Antidepressants (e.g., amitriptyline) for neuropathic pain
- Anticonvulsants (e.g., gabapentin, pregabalin) to calm nerve activity
- NMDA receptor antagonists (in refractory cases)
- Non-Drug Therapies:
- Mirror Therapy: Uses visual feedback to retrain the brain and reduce pain perception
- Transcutaneous Electrical Nerve Stimulation (TENS): Electrical pulses applied to the stump to reduce nerve pain
- Cognitive Behavioral Therapy (CBT): To manage emotional distress and coping
- Biofeedback & Meditation: Used in integrative medicine centers for mind-body regulation
- Advanced Interventions:
- Spinal cord stimulation and nerve blocks offered in major hospitals
- Virtual reality therapy (emerging in Korean rehabilitation medicine)
- Prosthetics with sensory feedback technology under clinical development
- Specialist Facilities:
- Leading Korean hospitals like Seoul National University Hospital, Asan Medical Center, and National Rehabilitation Center (Seoul) offer expert care in amputee rehabilitation and chronic pain management.
- Services include interdisciplinary teams of pain specialists, physiatrists, occupational therapists, and psychologists.