Overview
Persistent Pulmonary Hypertension of the Newborn (PPHN) is a life-threatening condition that affects newborns shortly after birth. It occurs when a baby’s circulation system fails to adapt to breathing outside the womb, causing high pressure in the lungs’ blood vessels and reducing oxygen flow into the bloodstream. Immediate medical intervention in a neonatal intensive care unit (NICU) is essential for survival and long-term health.
What is Persistent Pulmonary Hypertension of the Newborn?
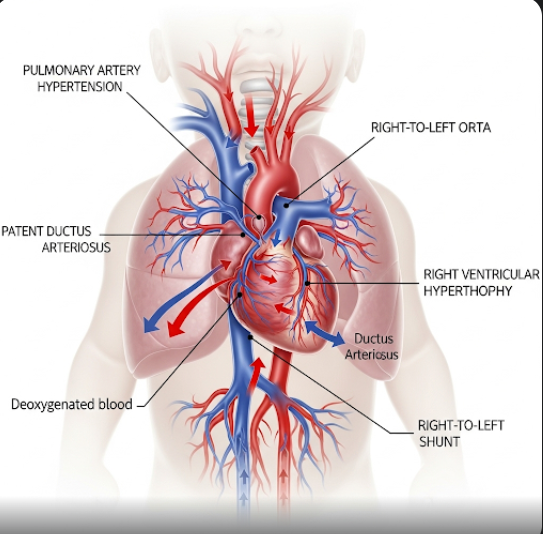
PPHN is a disorder where the newborn’s blood vessels in the lungs remain constricted after birth, leading to elevated pulmonary artery pressure. In a healthy newborn, blood flow transitions from the fetal pattern (which bypasses the lungs) to normal postnatal circulation. In PPHN, this transition doesn’t occur correctly, so oxygen-poor blood bypasses the lungs and circulates through the body, leading to severe hypoxemia (low blood oxygen levels). This condition mimics persistent fetal circulation and is considered a medical emergency.
Symptoms
PPHN symptoms typically develop within the first hours after birth and may include:
- Severe cyanosis (bluish skin or lips)
- Rapid breathing (tachypnea)
- Low oxygen levels despite oxygen therapy
- Lethargy or poor feeding
- Low blood pressure (hypotension)
- Heart murmur or abnormal heart sounds
- Cool extremities or delayed capillary refill
- Signs of respiratory distress, such as nasal flaring, grunting, or chest retractions
In many cases, standard oxygen therapy does not improve the baby’s oxygen levels, indicating a need for specialized care.
Causes
Several underlying conditions or perinatal events can trigger PPHN, including:
- Meconium aspiration syndrome
- Neonatal sepsis or pneumonia
- Birth asphyxia (lack of oxygen during delivery)
- Pulmonary hypoplasia (underdeveloped lungs)
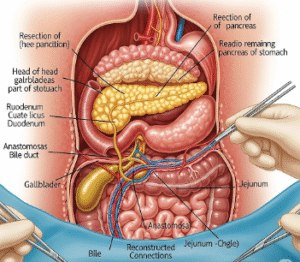
- Diaphragmatic hernia
- Maternal use of non-steroidal anti-inflammatory drugs (NSAIDs) late in pregnancy
- Premature closure of the ductus arteriosus in utero
The condition can also be idiopathic, meaning no specific cause is identified.
Risk Factors
PPHN is more likely to occur in newborns with the following risk factors:
- Full-term or post-term birth
- Cesarean delivery without labor
- Low Apgar scores at birth
- Maternal diabetes or obesity
- Intrauterine growth restriction (IUGR)
- Exposure to certain medications in utero
- Male infants (statistically higher incidence)
Complications
Without prompt and effective treatment, PPHN can lead to serious health issues:
- Severe hypoxemia leading to organ failure
- Developmental delays or neurological damage due to prolonged oxygen deprivation
- Hearing loss (observed in up to 30% of cases)
- Cardiopulmonary arrest
- Death, especially if not diagnosed or managed in time
Survivors may also face long-term respiratory or neurodevelopmental challenges.
Prevention
While not all cases are preventable, certain steps can reduce the risk:
- Adequate prenatal care and monitoring high-risk pregnancies
- Avoiding NSAIDs or harmful medications late in pregnancy
- Early treatment of maternal infections or health conditions
- Careful monitoring during labor and delivery
- Proper neonatal resuscitation at birth for babies at risk
- Delay of elective cesarean sections until at least 39 weeks unless medically necessary
Treatment Options in Korea
South Korea is internationally recognized for its advanced neonatal care, and NICUs in top-tier hospitals provide cutting-edge treatment for PPHN. Treatment strategies include:
- Supplemental Oxygen: Delivered via mechanical ventilation or continuous positive airway pressure (CPAP) to assist breathing.
- Inhaled Nitric Oxide (iNO): A key therapy that helps dilate pulmonary blood vessels and improve oxygenation without causing systemic hypotension.
- High-Frequency Ventilation: Used for babies with severe lung problems to provide oxygenation with minimal lung injury.
- Extracorporeal Membrane Oxygenation (ECMO): Available in Korea’s leading NICUs for severe cases, ECMO temporarily takes over heart and lung functions, allowing the baby’s organs to rest and recover.
- Sedation and Supportive Care: To reduce stress and oxygen demand.
- Medications: Sildenafil and milrinone may be used to relax pulmonary vessels and support heart function.
- Multidisciplinary Monitoring: Continuous assessment by neonatologists, pediatric cardiologists, and respiratory therapists.
Major hospitals such as Samsung Medical Center, Severance Hospital, Asan Medical Center, and Seoul National University Children’s Hospital have top-tier NICUs equipped with advanced technology and expert staff experienced in managing PPHN cases with excellent outcomes.