Overview
Persistent Fetal Circulation, also known as Persistent Pulmonary Hypertension of the Newborn (PPHN), is a serious neonatal condition in which a newborn’s circulation continues to follow the fetal pattern after birth, preventing normal oxygenation of the blood. It can lead to severe hypoxemia (low blood oxygen levels) and respiratory distress shortly after delivery. Immediate diagnosis and treatment are crucial to prevent life-threatening complications.
What is Persistent Fetal Circulation?
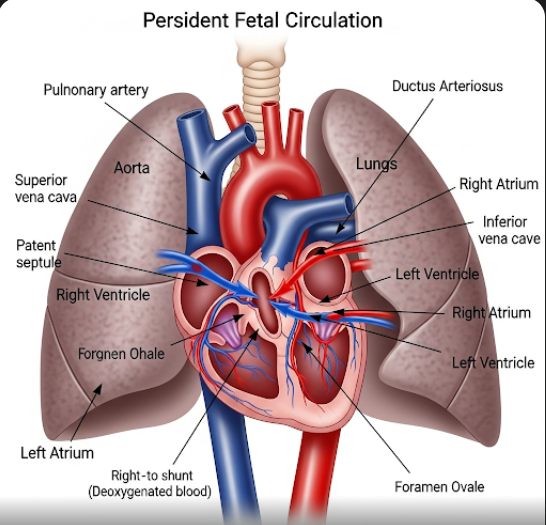
Before birth, a fetus relies on the placenta—not the lungs—for oxygen exchange. In this fetal circulation, blood bypasses the lungs via two main shunts: the ductus arteriosus and foramen ovale. Normally, after birth, these shunts close as the lungs take over oxygen exchange. However, in Persistent Fetal Circulation, these pathways fail to close properly, and the pulmonary blood vessels remain constricted, resulting in blood continuing to bypass the lungs. This condition is categorized under neonatal pulmonary hypertension and requires urgent neonatal intensive care.
Symptoms
Signs of Persistent Fetal Circulation typically appear within the first 12–24 hours after birth and may include:
- Rapid breathing (tachypnea)
- Grunting or nasal flaring
- Cyanosis (bluish tint to the skin, lips, or nails)
- Low oxygen levels despite oxygen therapy
- Low blood pressure (hypotension)
- Cold extremities or poor circulation
- Enlarged heart or abnormal heart sounds (heard on echocardiography)
These symptoms often indicate respiratory distress and require immediate medical evaluation.
Causes
Persistent Fetal Circulation can occur as a primary condition or secondary to other perinatal complications. Common causes include:
- Birth asphyxia (lack of oxygen during delivery)
- Meconium aspiration syndrome
- Pneumonia or sepsis
- Lung hypoplasia (underdeveloped lungs)
- Diaphragmatic hernia
- Premature closure of the ductus arteriosus in utero
- Maternal use of non-steroidal anti-inflammatory drugs (NSAIDs) late in pregnancy
- High altitude births (due to naturally lower oxygen levels)
Risk Factors
Factors that increase the likelihood of Persistent Fetal Circulation include:
- Full-term or post-term birth
- Cesarean delivery (especially without labor)
- Maternal diabetes
- Maternal infection or chorioamnionitis
- Meconium-stained amniotic fluid
- Prolonged labor or difficult delivery
- Male infants (slightly higher risk)
Complications
If not treated promptly and effectively, PFC/PPHN can lead to severe complications, including:
- Severe hypoxemia and acidosis
- Multi-organ dysfunction (brain, kidneys, liver)
- Brain damage or developmental delays
- Hearing loss
- Cardiopulmonary arrest
- Neonatal death (in severe untreated cases)
Early intervention significantly reduces the risk of long-term effects.
Prevention
While not all cases can be prevented, steps to reduce the risk of PFC include:
- Proper prenatal care to monitor fetal well-being
- Avoiding late-pregnancy use of NSAIDs or other risky medications
- Prompt management of maternal infections or complications
- Careful monitoring during labor and delivery
- Immediate neonatal resuscitation if needed at birth
- Avoiding elective cesarean sections before 39 weeks without medical indication
Treatment Options in Korea
South Korea is well-equipped with modern neonatal intensive care units (NICUs) and advanced neonatal cardiopulmonary management systems for treating PFC. Common treatments include:
- Oxygen Therapy: High-concentration oxygen delivered via mechanical ventilation or CPAP to improve oxygenation.
- Mechanical Ventilation: To assist breathing and ensure adequate lung expansion.
- Inhaled Nitric Oxide (iNO): A specialized gas therapy that relaxes the pulmonary vessels and improves oxygenation without affecting systemic blood pressure.
- Extracorporeal Membrane Oxygenation (ECMO): Available in advanced Korean NICUs for life-threatening cases, ECMO temporarily takes over the function of the lungs and heart.
- Sedation and Fluid Management: To reduce stress on the newborn and stabilize blood pressure.
- Treatment of Underlying Causes: Infections are treated with antibiotics; meconium aspiration may require suction and intensive pulmonary support.
- Monitoring and Follow-up: Neonates receive continuous monitoring of oxygen levels, heart function, and development over time.
Top hospitals in Korea such as Seoul National University Hospital, Samsung Medical Center, Asan Medical Center, and Severance Children’s Hospital offer cutting-edge NICU care with excellent survival outcomes for newborns diagnosed with PFC.