Overview
Perinatal asphyxia is a serious medical condition that occurs when a newborn does not receive enough oxygen before, during, or immediately after birth. This oxygen deprivation can lead to brain damage, organ failure, and even death if not treated promptly. It is one of the leading causes of neonatal morbidity and mortality worldwide, particularly in low-resource settings. Early detection, rapid intervention, and supportive care are critical for improving outcomes.
What is Perinatal Asphyxia?
Perinatal asphyxia refers to a lack of oxygen (hypoxia) and/or impaired blood flow (ischemia) to a newborn’s brain and other vital organs around the time of birth. This oxygen shortage leads to an accumulation of carbon dioxide and acid in the blood (acidosis), causing cellular injury.
This condition can affect full-term or premature babies and may occur:
- Before birth (antenatal)
- During labor and delivery (intrapartum)
- Immediately after birth (postnatal)
In severe cases, perinatal asphyxia can result in Hypoxic-Ischemic Encephalopathy (HIE)—a type of brain damage due to oxygen deprivation.
Symptoms
Signs of perinatal asphyxia may appear at birth or within hours after delivery. Common symptoms include:
- Low Apgar score (less than 7 at 5 minutes)
- Weak or absent breathing
- Poor muscle tone or limp body
- Blue or pale skin (cyanosis)
- Abnormal heart rate
- Seizures
- Low blood pressure
- Decreased responsiveness
- Organ dysfunction, such as kidney or liver problems
Newborns may also have difficulty feeding, irregular reflexes, or delayed development in the longer term.
Causes
Perinatal asphyxia is often caused by factors that interfere with the baby’s oxygen supply during the perinatal period. Common causes include:
Before birth:
- Placental abruption (early separation from the uterus)
- Umbilical cord compression or prolapse
- Maternal hypotension or shock
- Severe intrauterine growth restriction (IUGR)
- Maternal infections
- Chronic fetal distress
During labor/delivery:
- Prolonged or difficult labor
- Shoulder dystocia
- Breech presentation
- Inadequate fetal monitoring
- Uterine rupture
After birth:
- Delayed resuscitation
- Respiratory failure
- Congenital heart or lung defects
Risk Factors
Certain maternal, fetal, and delivery-related factors can increase the risk of perinatal asphyxia:
- Premature birth
- Maternal diabetes or high blood pressure
- Preeclampsia or eclampsia
- Prolonged labor or instrumental delivery
- Multiple gestation (twins, triplets)
- Previous stillbirth or high-risk pregnancy
- Lack of access to skilled birth attendants
- Inadequate prenatal care
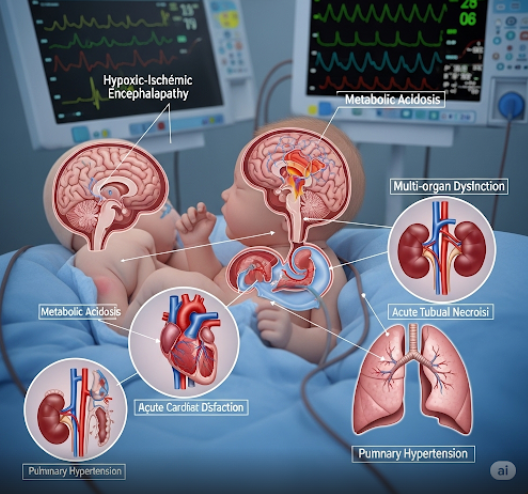
Complications
Perinatal asphyxia can have devastating short-term and long-term consequences:
Immediate complications:
- Hypoxic-Ischemic Encephalopathy (HIE)
- Respiratory distress syndrome (RDS)
- Seizures
- Multi-organ dysfunction (heart, kidneys, liver)
- Death within hours or days
Long-term complications:
- Cerebral palsy
- Developmental delay
- Intellectual disability
- Epilepsy
- Vision or hearing problems
- Behavioral and learning disorders
The severity of complications depends on the duration and degree of oxygen deprivation and how quickly treatment is initiated.
Prevention
While not all cases can be prevented, several strategies can reduce the risk of perinatal asphyxia:
- Regular prenatal care to monitor fetal well-being
- Early detection of high-risk pregnancies
- Effective management of maternal conditions (e.g., hypertension, diabetes)
- Skilled attendance at birth by trained obstetric and neonatal staff
- Continuous fetal monitoring during labor
- Timely cesarean delivery when necessary
- Immediate neonatal resuscitation if signs of asphyxia are present
- Educating healthcare teams on emergency protocols and best practices
Treatment Options in Korea
South Korea offers advanced neonatal care, including modern NICUs and high-survival rates for asphyxiated infants. Treatment focuses on stabilizing the baby, minimizing brain injury, and supporting recovery.
Initial Resuscitation:
- Clearing airways and establishing breathing
- Oxygen administration and ventilation
- Chest compressions and medications if needed
Hospital Care:
- NICU monitoring with full life support
- Therapeutic hypothermia (cooling therapy) within 6 hours of birth to reduce brain damage
- Mechanical ventilation for breathing support
- Intravenous fluids, electrolytes, and medications to support organs
- Seizure control with anticonvulsants
- MRI or brain scans to assess HIE or other damage
- Early rehabilitation (physical, occupational, and speech therapy) if developmental delays are suspected
Leading Hospitals in Korea:
Top medical centers like Seoul National University Hospital, Asan Medical Center, Samsung Medical Center, and Severance Hospital provide 24/7 neonatal intensive care, cutting-edge technology, and internationally trained specialists. Korean NICUs are equipped with therapeutic hypothermia systems, neuro-monitoring, and family-centered care programs.