Overview
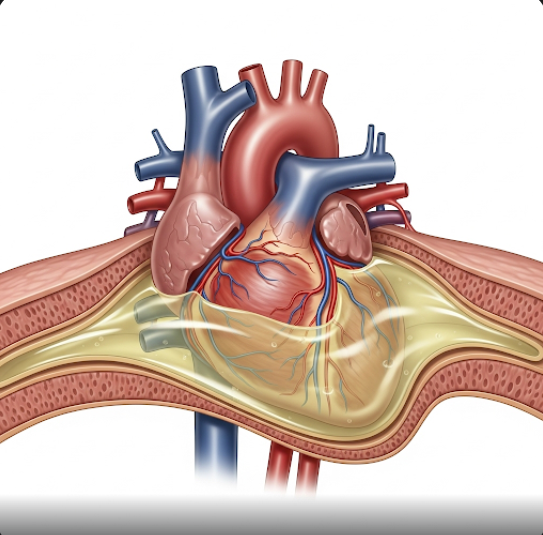
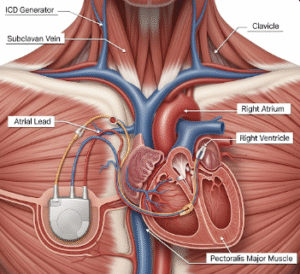
Pericardial effusion is a medical condition in which excess fluid accumulates in the pericardial sac, the thin, double-layered membrane that surrounds the heart. While a small amount of fluid is normally present to reduce friction during heartbeats, an abnormal build-up can compress the heart and interfere with its ability to pump blood. In severe cases, this condition can progress to cardiac tamponade, a life-threatening emergency requiring urgent treatment.
What is Pericardial Effusion?
Pericardial effusion occurs when fluid builds up between the visceral and parietal layers of the pericardium. This can be caused by inflammation (pericarditis), infection, trauma, cancer, autoimmune conditions, or as a complication of surgery.
The condition may be:
- Acute: Rapid onset, often more dangerous
- Chronic: Slow accumulation over time, possibly asymptomatic
- Small, moderate, or large, depending on the volume of fluid
Mild effusions may resolve on their own, while larger ones may impair cardiac function and require drainage.
Symptoms
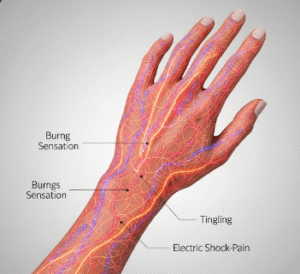
Symptoms depend on the volume and speed of fluid accumulation and may range from none to severe:
- Chest pain or pressure, often sharp or worsened by breathing or lying down
- Shortness of breath, especially when reclining
- Fatigue or weakness
- Lightheadedness or dizziness
- Palpitations or irregular heartbeat
- Low blood pressure
- Swelling in the legs or abdomen
- Cough or hoarseness (from compression of nearby structures)
- In severe cases: fainting or shock (signs of cardiac tamponade)
Causes
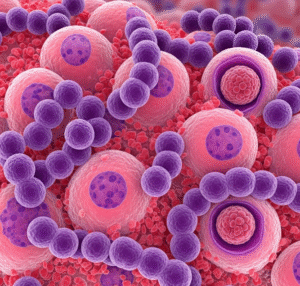
Pericardial effusion can result from various underlying conditions or events:
- Pericarditis (inflammation of the pericardium)
- Infections: Viral (e.g., Coxsackievirus), bacterial (e.g., tuberculosis), fungal
- Cancer, especially lung or breast cancer, lymphoma, or metastasis to the pericardium
- Trauma or injury, including surgery or chest injury
- Autoimmune diseases, such as lupus, rheumatoid arthritis, or scleroderma
- Kidney failure (uremic pericarditis)
- Hypothyroidism
- Radiation therapy to the chest
- Use of certain medications, such as hydralazine or isoniazid
In some cases, the cause may be idiopathic (unknown).
Risk Factors
You may be at greater risk of developing pericardial effusion if you:
- Have had recent heart surgery or trauma
- Have a history of cancer (especially lung or breast)
- Are undergoing chemotherapy or radiation
- Have chronic kidney disease or are on dialysis
- Have an autoimmune disorder
- Suffer from untreated infections, especially in endemic regions (e.g., tuberculosis)
- Take certain medications that can cause pericarditis as a side effect
Complications
If not diagnosed and treated, pericardial effusion can lead to:
- Cardiac tamponade: A critical condition where the pressure from fluid buildup prevents the heart from filling properly, leading to a drop in blood pressure and shock
- Constrictive pericarditis: Scarring and thickening of the pericardium, causing chronic heart dysfunction
- Heart failure
- Severe arrhythmias
- Death, in cases of untreated tamponade
Prompt medical attention is essential if symptoms suggest complications.
Prevention
While not all cases of pericardial effusion can be prevented, especially those due to cancer or autoimmune diseases, the following strategies can help reduce risk:
- Treat infections early and completely
- Manage chronic illnesses like kidney disease, lupus, or rheumatoid arthritis
- Monitor for pericardial symptoms after heart surgery or trauma
- Avoid known medication triggers if previously affected
- Get regular check-ups if you are at risk due to past medical history
- Vaccinate against viruses (e.g., influenza, COVID-19) to reduce post-viral pericarditis risk
Treatment Options in Korea
South Korea offers world-class cardiovascular care, including specialized diagnostics and treatment for pericardial effusion. Treatment depends on the cause, severity, and symptoms.
Diagnosis:
- Echocardiogram (ultrasound of the heart): Primary tool for detecting fluid volume and pressure
- Electrocardiogram (ECG): May show changes related to pericarditis or tamponade
- Chest X-ray and CT or MRI scans: Assess heart size and structure
- Pericardiocentesis (fluid analysis): To identify the cause (infection, malignancy, inflammation)
- Blood tests: To detect infection, autoimmune markers, or thyroid/kidney problems
Treatment Options:
- Observation: Small, asymptomatic effusions may resolve on their own
- Medications:
- NSAIDs or colchicine for inflammation
- Antibiotics for bacterial infection
- Corticosteroids or immunosuppressants for autoimmune causes
- Diuretics for fluid control if associated with heart failure
- Pericardiocentesis: Needle drainage of fluid for large or symptomatic effusions
- Pericardial window surgery: Creates a drainage passage for recurrent effusions
- Pericardiectomy (removal of pericardium): For chronic or constrictive cases
Where to Get Treated in Korea:
Leading cardiac centers such as Asan Medical Center, Seoul National University Hospital, Samsung Medical Center, and Severance Hospital offer 24/7 emergency care, advanced imaging, and surgical treatment for pericardial diseases. These hospitals also provide multilingual support for international patients.