Overview
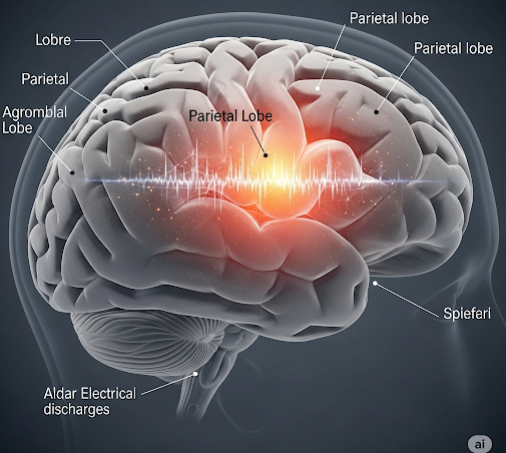
Parietal lobe epilepsy is a rare and complex form of focal epilepsy that originates in the parietal lobe of the brain, which is responsible for processing sensory information like touch, spatial orientation, and body awareness. Because of the region’s functions, seizures in this area can produce unusual sensory disturbances, such as tingling, numbness, or feelings of disconnection from the body. Diagnosis is challenging due to the variability of symptoms, but advancements in neuroimaging and electroencephalography (EEG) have improved its detection and treatment.
What is Parietal Lobe Epilepsy?
Parietal lobe epilepsy is a type of focal (partial) epilepsy where the seizure activity starts in the parietal lobe of the brain. This form of epilepsy is much less common than seizures originating in the temporal or frontal lobes. It may cause atypical sensory experiences, including feelings of distortion in body image, hallucinations of touch, or the sensation of movement when none exists.
Because the parietal lobe connects with multiple other brain regions, seizures may quickly spread, sometimes making it hard to distinguish their point of origin.
Symptoms
Symptoms of parietal lobe epilepsy depend on the specific area of the parietal lobe affected. Common symptoms include:
- Tingling or numbness in a specific part of the body
- Distorted body image (e.g., limbs feeling larger or smaller)
- Visual distortions or hallucinations
- Auditory symptoms in some cases
- Feelings of déjà vu or jamais vu
- Motor symptoms if the seizure spreads to adjacent lobes
- Confusion or disorientation post-seizure
- Sometimes loss of consciousness, but not always
Seizures may last from seconds to a few minutes and can be followed by fatigue or confusion.
Causes
Several underlying issues can lead to parietal lobe epilepsy, including:
- Brain injuries or trauma affecting the parietal lobe
- Brain tumors or lesions
- Cortical dysplasia (abnormal brain development)
- Stroke or reduced blood flow to the parietal region
- Infections such as encephalitis or meningitis
- Neurodegenerative conditions
- Genetic predispositions (in rare cases)
In some instances, the cause remains idiopathic, meaning it is unknown despite thorough testing.
Risk Factors
Risk factors for developing parietal lobe epilepsy include:
- History of head trauma or concussions
- Family history of epilepsy or seizure disorders
- Previous neurological infections
- Brain surgery or tumors in or near the parietal lobe
- Congenital brain malformations
- Stroke survivors
- Exposure to toxins or drugs that impact brain function
Children and young adults are often more susceptible to epilepsy onset, though it can occur at any age.
Complications
If left untreated or poorly managed, parietal lobe epilepsy may lead to:
- Increased seizure frequency or severity
- Seizure-related injuries, especially during complex or generalized seizures
- Cognitive decline, especially if seizures are frequent or prolonged
- Mental health issues, such as anxiety or depression
- Social challenges, including fear of public episodes
- Status epilepticus, a life-threatening condition where seizures last too long or occur too frequently without recovery between them
Prevention
While not all forms of epilepsy can be prevented, the following steps can reduce risk or improve early detection:
- Protect the head during physical activities to prevent trauma
- Manage chronic conditions like high blood pressure and diabetes to lower stroke risk
- Seek treatment for any brain infections or tumors early
- Avoid substance abuse that can harm brain tissue
- Undergo regular checkups if you have a family history of neurological disorders
- Medication adherence if already diagnosed to prevent worsening
- Consider genetic counseling if epilepsy runs in the family
Treatment Options in Korea
South Korea is at the forefront of epilepsy diagnosis and treatment, offering advanced medical solutions and personalized care plans.
1. Diagnostic Tools
- Electroencephalogram (EEG): to monitor electrical activity in the brain
- MRI or CT scans: to locate any brain abnormalities
- PET and SPECT scans: for brain mapping and seizure localization
- Video EEG monitoring: in epilepsy centers for detailed observation
2. Medical Treatment
- Antiepileptic drugs (AEDs): including levetiracetam, lamotrigine, or carbamazepine
- Dosages are personalized based on seizure type and frequency
- Regular neurologist follow-up to adjust medication
3. Surgical Treatment
- For patients resistant to medications, epilepsy surgery may be considered
- Resective surgery: removal of seizure-causing brain tissue
- Responsive neurostimulation (RNS) or vagus nerve stimulation (VNS) for those not eligible for resection
4. Lifestyle & Supportive Care
- Dietary therapies like the ketogenic diet
- Psychological counseling to manage emotional stress
- Rehabilitation services to address cognitive or physical effects of seizures
- Seizure alert systems and wearable technology for monitoring
5. Leading Hospitals in Korea
- Severance Hospital (Yonsei University)
- Samsung Medical Center
- Asan Medical Center
- Seoul National University Hospital
These institutions offer English-speaking neurology teams, international patient support, and cutting-edge epilepsy care, making Korea a sought-after destination for global epilepsy treatment.