Overview
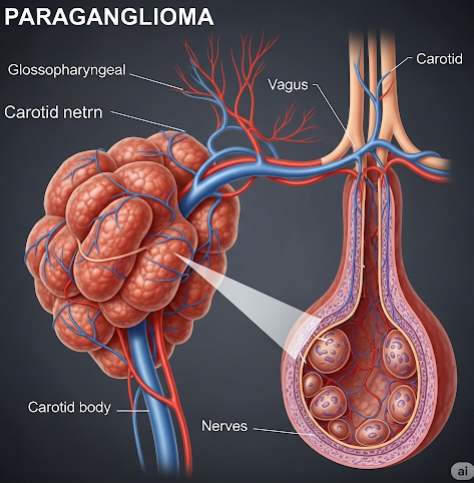
Paraganglioma is a rare type of neuroendocrine tumor that develops from paraganglionic tissue, a group of cells that originate from the nervous system and help regulate involuntary functions like blood pressure. These tumors can form in various parts of the body, including the head, neck, chest, abdomen, and pelvis. While many paragangliomas are non-cancerous (benign), some can become malignant and spread to other parts of the body. Early diagnosis and treatment are essential for a favorable outcome.
What is Paraganglioma?
Paragangliomas are tumors that arise from extra-adrenal chromaffin cells, which are located outside the adrenal glands. They are closely related to pheochromocytomas, which are similar tumors found in the adrenal glands. Paragangliomas can be categorized based on their location:
- Sympathetic paragangliomas: Often located in the chest, abdomen, or pelvis and may produce hormones like adrenaline.
- Parasympathetic paragangliomas: Typically found in the head and neck region and are usually nonfunctional (do not produce hormones).
Some paragangliomas produce excessive catecholamines (stress hormones), causing symptoms like high blood pressure, rapid heartbeat, and sweating.
Symptoms
Symptoms vary depending on tumor location and whether it secretes hormones:
Functional (hormone-producing) paragangliomas:
- High blood pressure (hypertension)
- Rapid heartbeat (tachycardia)
- Excessive sweating
- Headaches
- Anxiety or panic-like symptoms
- Tremors
- Palpitations
Nonfunctional (non-hormone-producing) paragangliomas:
- A painless lump or mass (in head, neck, or abdomen)
- Hoarseness or difficulty swallowing (for neck tumors)
- Hearing loss or ringing in ears (if near auditory nerves)
- Abdominal pain or discomfort
Causes
The exact cause of paragangliomas is often unknown, but many cases are linked to genetic mutations. In fact, up to 30-40% of patients have inherited genetic syndromes that increase the risk of developing these tumors. Common associated genetic conditions include:
- Multiple endocrine neoplasia (MEN) type 2
- Von Hippel-Lindau (VHL) disease
- Neurofibromatosis type 1 (NF1)
- Succinate dehydrogenase (SDH) gene mutations
Environmental factors are not well-established contributors to the disease.
Risk Factors
Risk factors for developing paraganglioma include:
- Family history of paraganglioma or pheochromocytoma
- Inherited genetic conditions (e.g., VHL, MEN2, SDH mutations)
- Age (commonly diagnosed in people between 30–50 years)
- Exposure to high-altitude environments (in some head/neck types)
- Previous radiation therapy to the head or neck (rare cases)
Complications
Potential complications of paraganglioma include:
- Hormonal crises: Sudden release of catecholamines can cause hypertensive crisis or cardiac arrhythmias.
- Metastasis: Although rare, some paragangliomas can become cancerous and spread to lungs, bones, or liver.
- Compression of nearby structures: Tumors in the neck or skull base may affect nerves, causing speech, swallowing, or hearing problems.
- Recurrence: Even after successful removal, tumors may recur, particularly in inherited cases.
- Surgical risks: Surgery near critical nerves or blood vessels may result in nerve damage or bleeding.
Prevention
There is no guaranteed way to prevent paraganglioma, but steps can be taken to reduce risks and catch the disease early:
- Genetic testing and counseling for individuals with a family history
- Regular screening and imaging for those with known genetic mutations
- Monitoring blood pressure and other vital signs for early detection of hormonal activity
- Avoiding triggers like stress or stimulant medications if diagnosed with a functional tumor
Treatment Option in Korea
Korea offers advanced diagnostic tools and treatment for paragangliomas at leading hospitals, including Seoul National University Hospital, Asan Medical Center, and Samsung Medical Center. Treatment depends on tumor size, location, functionality, and whether it has spread.
1. Surgical Removal
- The primary treatment for localized tumors.
- Surgeons use precise techniques (such as robotic-assisted or minimally invasive surgery) to reduce complications, especially for skull base or neck tumors.
2. Medications for Functional Tumors
- Alpha-blockers and beta-blockers are used to control high blood pressure and heart rate before surgery.
- Medications may also help control symptoms in inoperable cases.
3. Radiation Therapy
- Used for non-resectable tumors or those near sensitive nerves or blood vessels.
- Stereotactic radiosurgery (Gamma Knife or CyberKnife) is available in Korea for head/neck tumors.
4. Chemotherapy or Targeted Therapy
- Used for metastatic or malignant cases.
- Korea follows global oncology protocols, and genetic mutation-based targeted therapies (e.g., tyrosine kinase inhibitors) are available in top cancer centers.
5. Regular Monitoring
- Lifelong follow-up with MRI/CT scans, biochemical tests, and genetic counseling is offered.
- Korea’s integrated digital health system ensures easy access to monitoring and specialty care.
6. Genetic Counseling Services
- Available in major medical centers for patients and families with inherited paraganglioma syndromes.