Overview
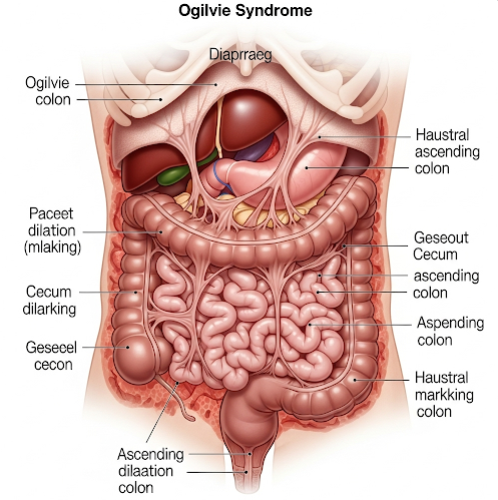
Ogilvie Syndrome, also known as acute colonic pseudo-obstruction (ACPO), is a rare but serious condition characterized by a sudden and severe dilation of the large intestine without any physical blockage. It typically affects hospitalized or critically ill patients, particularly after surgery or major illness. While it presents with symptoms similar to a mechanical bowel obstruction, no actual physical obstruction is found. Immediate medical attention is essential to prevent life-threatening complications such as bowel ischemia or perforation.
What is Ogilvie Syndrome?
Ogilvie Syndrome is a gastrointestinal disorder in which the colon becomes abnormally distended, especially in the cecum and ascending colon, without a clear mechanical cause. First described by Sir William Ogilvie in the 1940s, the condition results from a disruption in the autonomic nervous system’s control over bowel motility. This functional obstruction occurs most often in older adults who are recovering from serious illness, infection, or surgery.
Symptoms
Symptoms of Ogilvie Syndrome resemble those of a bowel blockage and may include:
- Noticeable abdominal swelling or bloating
- Abdominal pain or cramping
- Nausea and vomiting
- Constipation or inability to pass gas
- Decreased or absent bowel sounds
- Fever and signs of sepsis (in severe or advanced cases)
Causes
While the exact cause of Ogilvie Syndrome is not fully understood, it is thought to stem from an imbalance between sympathetic and parasympathetic nervous input to the colon. This results in impaired colonic motility. Common precipitating factors include:
- Major surgeries (especially orthopedic, abdominal, or pelvic)
- Severe infections
- Trauma
- Neurological disorders (e.g., Parkinson’s disease, multiple sclerosis)
- Electrolyte imbalances (especially potassium or magnesium)
- Certain medications (e.g., opioids, anticholinergics, calcium channel blockers)
Risk Factors
Individuals at higher risk for developing Ogilvie Syndrome include:
- Elderly patients, especially those over 60
- Patients recovering from major surgeries
- Individuals with chronic illnesses or prolonged immobility
- Those taking medications that affect bowel motility
- Patients in intensive care or those on mechanical ventilation
Complications
If not promptly diagnosed and treated, Ogilvie Syndrome can lead to:
- Bowel perforation (rupture of the colon)
- Peritonitis (inflammation of the abdominal lining)
- Sepsis (a life-threatening infection of the bloodstream)
- Bowel ischemia (loss of blood flow to the colon)
- Death (in severe untreated cases)
Prevention
While not all cases can be prevented, steps to reduce the risk include:
- Careful postoperative monitoring of bowel function
- Early mobilization after surgery or illness
- Avoiding unnecessary use of medications that slow gut motility
- Maintaining normal electrolyte levels
- Regular assessment of abdominal symptoms in high-risk patients
Treatment Options in Korea
South Korea offers advanced and efficient medical care for Ogilvie Syndrome, combining high-tech diagnostics with specialized gastrointestinal care. Treatment may include:
- Bowel rest and supportive care (e.g., IV fluids, electrolyte correction)
- Stopping medications that reduce bowel motility
- Decompression via rectal tubes or colonoscopy (for urgent relief of distention)
- Administration of neostigmine (a medication that stimulates bowel motility) under monitored conditions
- In severe or complicated cases, surgical intervention (e.g., cecostomy or resection)
Leading hospitals in Korea—such as Seoul National University Hospital, Asan Medical Center, and Samsung Medical Center—have multidisciplinary teams experienced in managing complex gastrointestinal conditions, including Ogilvie Syndrome.