Overview
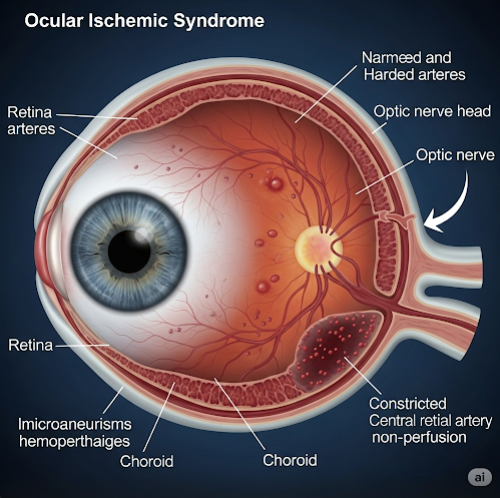
Ocular Ischemic Syndrome (OIS) is a rare but serious eye condition caused by insufficient blood flow to the eye, usually due to severe blockage or narrowing of the carotid artery, which supplies blood to the brain and eyes. This condition affects middle-aged and older adults, and it often signals advanced cardiovascular disease.
If not diagnosed and treated early, OIS can result in vision loss and may also indicate a high risk of stroke or heart attack.
What is Ocular Ischemic Syndrome?
OIS occurs when there is a chronic reduction of blood flow (ischemia) to the ocular structures, particularly the retina. This is typically caused by carotid artery stenosis (narrowing due to atherosclerosis), which decreases the perfusion pressure in the eye.
The reduced blood supply leads to retinal dysfunction, hemorrhages, and neovascularization, all of which threaten vision. It is often misdiagnosed as diabetic retinopathy, central retinal vein occlusion, or other retinal vascular diseases, delaying proper treatment.
Symptoms
Ocular Ischemic Syndrome may affect one or both eyes and usually presents gradually. Symptoms include:
- Gradual, painless vision loss (most common)
- Amaurosis fugax (temporary episodes of blindness in one eye)
- Eye pain or aching, especially with movement
- Redness of the eye
- Photophobia (light sensitivity)
- Floaters or flashes
- Prolonged recovery after exposure to bright light
- Double vision or blurred vision
- In advanced stages: total blindness
These symptoms are typically unilateral but may be bilateral in severe vascular disease.
Causes
The primary cause of OIS is severe atherosclerosis of the carotid arteries, especially when narrowing exceeds 70–90%. Other contributing causes may include:
- Carotid artery dissection
- Giant cell arteritis (inflammatory blood vessel disease)
- Thromboembolism
- Cardiac embolism
- Advanced hypertension or diabetes
The underlying issue is reduced perfusion pressure in the ophthalmic artery and retinal circulation, leading to hypoxia and ischemic damage.
Risk Factors
The risk of OIS increases in individuals with:
- Atherosclerosis and carotid artery disease
- Hypertension
- Diabetes mellitus
- Smoking history
- High cholesterol (hyperlipidemia)
- Coronary artery disease or peripheral artery disease
- Advanced age (typically over 50)
- History of transient ischemic attack (TIA) or stroke
OIS is often associated with systemic vascular compromise, so early identification is critical for life-saving interventions.
Complications
If left untreated, ocular ischemic syndrome can lead to:
- Permanent vision loss
- Neovascular glaucoma (due to abnormal blood vessel growth)
- Retinal or vitreous hemorrhage
- Central retinal artery or vein occlusion
- Ocular inflammation (uveitis or iritis)
- Increased risk of cerebrovascular accident (stroke)
- Increased risk of myocardial infarction (heart attack)
Because it signals widespread vascular disease, OIS is often a warning sign of systemic health emergencies.
Prevention
Preventing OIS involves controlling the underlying vascular risk factors:
- Regular cardiovascular checkups and carotid artery screening
- Managing hypertension, diabetes, and cholesterol levels
- Quitting smoking
- Healthy diet and regular exercise
- Taking prescribed blood thinners or statins, if needed
- Monitoring eye health, especially in patients with known vascular disease
Early detection of carotid artery narrowing can prevent OIS and reduce stroke risk.
Treatment Options in Korea
South Korea offers advanced interdisciplinary care involving ophthalmology, neurology, cardiology, and vascular surgery, making it a leading destination for diagnosing and managing OIS.
1. Diagnosis
- Dilated eye exam: To detect retinal hemorrhages, narrowed arteries, and neovascularization
- Fluorescein angiography: Shows delayed retinal blood flow
- Ocular Doppler ultrasound: Measures blood flow velocity in the eye
- Optical Coherence Tomography (OCT): Evaluates retinal thickness and ischemic damage
- Carotid Doppler ultrasound or CT/MR angiography: Confirms carotid artery stenosis
- Systemic evaluation: Blood pressure, glucose, cholesterol, and cardiac assessments
2. Medical Management
- Ocular pressure control: Eye drops for intraocular pressure
- Anti-VEGF injections: For neovascularization and macular edema
- Panretinal photocoagulation (PRP): Laser therapy to prevent abnormal vessel growth
- Anti-inflammatory or corticosteroid drops: For associated inflammation
3. Surgical and Vascular Intervention
- Carotid endarterectomy: Surgical removal of plaque from carotid artery
- Carotid artery stenting: Less invasive procedure to open narrowed arteries
- Management of systemic vascular conditions (e.g., bypass surgery, pacemaker for cardiac issues)
4. Multidisciplinary Care
- Coordinated treatment between ophthalmologists, neurologists, and vascular surgeons
- Monitoring for stroke prevention and vision preservation
5. Leading Hospitals in Korea for OIS and Vascular Eye Diseases
- Seoul National University Hospital – Neuro-Ophthalmology and Stroke Center
- Asan Medical Center – Department of Ophthalmology and Vascular Surgery
- Samsung Medical Center – Retinal & Vascular Eye Clinic
- Severance Hospital (Yonsei University) – Eye and Brain Hospital
- Korea University Anam Hospital – Carotid Disease and Ocular Stroke Unit
These hospitals offer:
- State-of-the-art imaging and surgical tools
- Rapid carotid screening and vascular intervention
- Multilingual services for international patients
- Long-term follow-up for stroke and vision protection