Overview
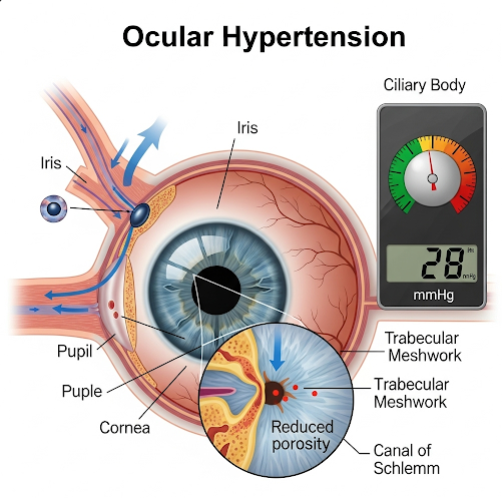
Ocular hypertension refers to a condition where the intraocular pressure (IOP) inside the eye is higher than normal, but without any signs of glaucoma, such as optic nerve damage or vision loss. It is not a disease in itself but a major risk factor for glaucoma, especially primary open-angle glaucoma.
People with ocular hypertension may not have any symptoms, which is why regular eye exams are essential for early detection and prevention of progression to glaucoma.
What is Ocular Hypertension?
Ocular hypertension occurs when the aqueous humor (the fluid inside the eye) is produced in excess or doesn’t drain properly, leading to increased pressure within the eye. Normal IOP ranges from 10 to 21 mmHg. In ocular hypertension, the pressure typically exceeds 21 mmHg.
While not everyone with ocular hypertension develops glaucoma, those with this condition are at a higher risk and may require monitoring or preventive treatment.
Symptoms
Most people with ocular hypertension do not experience any symptoms. It is often discovered during a routine eye exam. In some cases, if the pressure becomes very high, a person might experience:
- Eye discomfort or ache
- Headache
- Blurry vision (rare in mild cases)
- Halos around lights (if pressure is significantly elevated)
Because symptoms are typically absent, screening is crucial, especially for people at risk.
Causes
Ocular hypertension can be caused by an imbalance between the production and drainage of aqueous humor in the eye. Common causes include:
- Increased fluid production in the eye
- Decreased outflow or drainage of fluid through the trabecular meshwork
- Eye trauma or injury
- Steroid medication use, including eye drops
- Underlying eye conditions, such as pigment dispersion syndrome
- Age-related changes in the eye’s fluid dynamics
Risk Factors
Several factors increase the risk of developing ocular hypertension:
- Age over 40 years
- Family history of glaucoma
- African, Asian, or Hispanic descent
- Thinner corneas (central corneal thickness)
- Use of corticosteroids (especially long-term)
- High myopia (nearsightedness)
- Eye trauma or surgery
- Diabetes or high blood pressure
- Obstructive sleep apnea
If you fall into any of these categories, regular eye pressure monitoring is important.
Complications
If left untreated, ocular hypertension may lead to:
- Primary open-angle glaucoma
- Optic nerve damage
- Peripheral vision loss
- Total vision loss in severe cases
- Increased risk of ocular emergencies (e.g., acute angle-closure glaucoma)
Once glaucoma develops, vision loss is irreversible, so early detection of high eye pressure is key.
Prevention
While ocular hypertension itself may not always be preventable, the risk of progression to glaucoma can be minimized through:
- Regular comprehensive eye exams (every 1-2 years)
- Avoiding unnecessary steroid use
- Wearing eye protection to prevent injury
- Managing systemic health conditions like diabetes and hypertension
- Monitoring IOP if on long-term medications known to affect eye pressure
- Maintaining a healthy lifestyle (exercise, diet)
Early identification and risk assessment are essential to protect vision.
Treatment Options in Korea
South Korea offers cutting-edge care in the management of ocular hypertension through specialized ophthalmology clinics and eye hospitals.
1. Diagnosis
- Tonometry: Measures intraocular pressure (non-contact or applanation)
- Ophthalmoscopy: Examines the optic nerve
- Visual field test (perimetry): Checks for peripheral vision loss
- Optical Coherence Tomography (OCT): Monitors nerve fiber layer thickness
- Pachymetry: Measures corneal thickness (important for accurate IOP assessment)
- Gonioscopy: Evaluates the drainage angle inside the eye
2. Monitoring (No Immediate Treatment)
In mild cases with low risk, doctors may recommend:
- Regular eye pressure checks
- Visual field monitoring
- Lifestyle adjustments
- Education on glaucoma warning signs
3. Medication Therapy
If treatment is needed, the most common approach includes:
- Prostaglandin analogs (e.g., latanoprost): Increase fluid outflow
- Beta-blockers (e.g., timolol): Reduce fluid production
- Alpha agonists and carbonic anhydrase inhibitors: Other options for lowering IOP
- Fixed-combination eye drops: Combine two medications for better control
4. Laser or Surgical Intervention
For high-risk or non-responsive cases:
- Laser trabeculoplasty: Improves fluid drainage
- Minimally invasive glaucoma surgery (MIGS)
- Conventional filtering surgery (e.g., trabeculectomy)
5. Leading Eye Hospitals in Korea
- Severance Eye Hospital (Yonsei University) – Glaucoma and IOP Clinic
- Samsung Medical Center – Department of Ophthalmology
- Asan Medical Center – Advanced Glaucoma Services
- Seoul National University Hospital – Vision and Optic Nerve Clinic
- Kim’s Eye Hospital – Glaucoma Center
These facilities offer:
- Accurate pressure monitoring and imaging
- Advanced laser and surgical treatments
- Customized care for high-risk patients
- Multilingual services for international patients