Overview
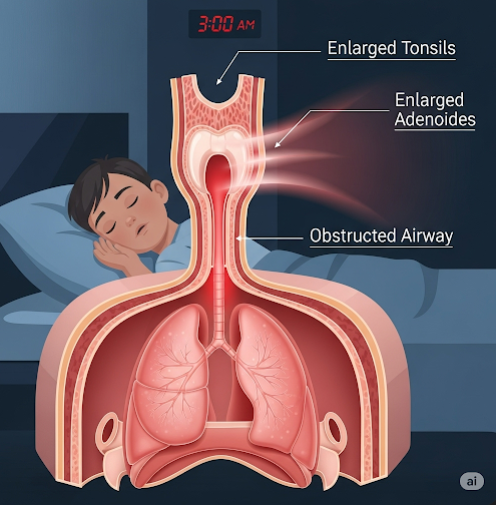
Obstructive Sleep Apnea (OSA) in children is a sleep disorder where a child’s breathing is partially or completely blocked repeatedly during sleep due to airway obstruction. Unlike adult OSA, which is often related to obesity, in children, the most common cause is enlarged tonsils or adenoids. OSA can lead to poor growth, behavioral issues, learning difficulties, and cardiovascular complications if untreated.
It is estimated that 1% to 5% of children suffer from OSA, and it is most common between the ages of 2 and 8 years.
What is Obstructive Sleep Apnea in Children?
Pediatric OSA is a type of sleep-disordered breathing (SDB) that occurs when muscles in the throat relax during sleep, causing soft tissues to collapse and block the airway. This leads to:
- Interrupted sleep
- Decreased oxygen levels
- Frequent nighttime awakenings
Because children may not always appear sleepy during the day, the condition is often misdiagnosed as behavioral problems or ADHD.
Symptoms
Symptoms of OSA in children can be both nighttime and daytime in nature:
Nighttime symptoms:
- Loud, frequent snoring
- Pauses in breathing or gasping
- Restless sleep or frequent position changes
- Sweating during sleep
- Mouth breathing or dry mouth in the morning
- Bedwetting (especially after age 5)
- Sleepwalking or night terrors
Daytime symptoms:
- Hyperactivity or inattentiveness
- Poor academic performance
- Irritability or mood swings
- Morning headaches
- Fatigue or sleepiness (especially in older children)
- Delayed growth or weight gain
If untreated, OSA can affect both physical and brain development.
Causes
The most common causes of OSA in children include:
- Enlarged tonsils and adenoids: The leading cause
- Obesity (in older children and adolescents)
- Nasal allergies or chronic congestion
- Craniofacial abnormalities (e.g., small jaw, cleft palate)
- Neuromuscular conditions (e.g., cerebral palsy)
- Genetic syndromes (e.g., Down syndrome, Pierre Robin sequence)
Airway obstruction can be temporary or chronic, depending on the cause.
Risk Factors
Children are at increased risk for OSA if they have:
- Large tonsils or adenoids
- Obesity or rapid weight gain
- Family history of sleep apnea
- Asthma or chronic nasal allergies
- Neurological or muscular disorders
- Craniofacial structural differences
- Prematurity or low birth weight
Children with Down syndrome and Prader-Willi syndrome are at particularly high risk.
Complications
Untreated pediatric OSA can lead to serious complications, including:
- Behavioral problems and learning disabilities
- Delayed growth and development
- Heart problems (e.g., pulmonary hypertension, right heart strain)
- High blood pressure
- Poor quality of life for the child and family
- Obesity or metabolic issues in older children
In severe cases, OSA can also impact speech development and cognitive function.
Prevention
While not all cases of OSA are preventable, you can reduce the risk through:
- Managing allergies and nasal congestion
- Promoting a healthy weight with diet and exercise
- Encouraging nose breathing over mouth breathing
- Avoiding exposure to tobacco smoke
- Monitoring children with craniofacial or neurological conditions closely
Early recognition and treatment are essential to prevent long-term effects.
Treatment Options in Korea
South Korea has advanced pediatric care and sleep medicine centers, offering world-class treatment for children with OSA.
1. Diagnosis
- Pediatric sleep study (polysomnography): Gold standard test
- ENT examination: To assess tonsils, adenoids, nasal structures
- Allergy testing and imaging (X-rays, CT scan if needed)
- Questionnaires for sleep habits and behavior
2. Non-Surgical Treatment
- Nasal corticosteroids or antihistamines (for allergies)
- Weight management programs (if obesity is a factor)
- CPAP (Continuous Positive Airway Pressure) in moderate-to-severe cases when surgery is not an option
- Myofunctional therapy: Exercises to improve airway muscle tone
- Behavioral therapy for associated ADHD-like symptoms
3. Surgical Treatment
- Tonsillectomy and/or adenoidectomy (T&A): First-line treatment for most children
- Orthodontic interventions: Such as rapid maxillary expansion for structural airway narrowing
- Tracheostomy or other advanced surgery (rare, for severe or complex cases)
4. Multidisciplinary Pediatric Sleep Centers in Korea
Top hospitals with pediatric sleep apnea expertise include:
- Severance Hospital (Yonsei University) – Pediatric Sleep Clinic
- Asan Medical Center – Department of Pediatric ENT and Sleep Medicine
- Seoul National University Hospital – Pediatric Pulmonology and ENT
- Samsung Medical Center – Pediatric Sleep and Breathing Disorders Clinic
- CHA Bundang Medical Center – Child Development and Sleep Clinic
These centers offer:
- Child-friendly sleep labs
- ENT and pediatric pulmonologist collaboration
- Parental counseling and follow-up care
- Multilingual support for international patients