Overview
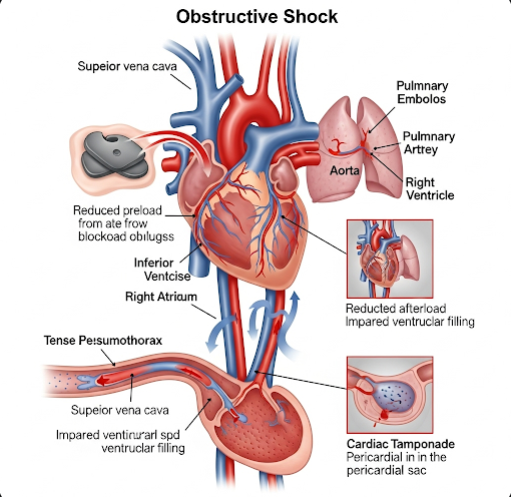
Obstructive shock is a rare but life-threatening condition that occurs when there is a mechanical obstruction to blood flow, preventing oxygen-rich blood from reaching vital organs. Even if the heart is functioning properly, this blockage causes a dramatic drop in blood pressure and tissue perfusion, leading to organ failure if not treated quickly.
Unlike other types of shock (such as hypovolemic, cardiogenic, or distributive), obstructive shock is caused by physical interference with the heart or great vessels, most often due to trauma, embolism, or cardiac tamponade. Immediate recognition and intervention are critical for survival.
What is Obstructive Shock?
Obstructive shock is one of the four main types of circulatory shock, characterized by impaired cardiac output due to a mechanical obstruction in the circulatory system. Despite adequate blood volume and cardiac function, blood cannot effectively circulate due to an external or internal blockage.
Common causes include:
- Tension pneumothorax
- Cardiac tamponade
- Massive pulmonary embolism (PE)
- Severe aortic stenosis or dissection
- Intrathoracic tumors or abdominal compartment syndrome
If not reversed promptly, obstructive shock leads to hypoxia, lactic acidosis, multi-organ failure, and death.
Symptoms
Symptoms of obstructive shock can appear rapidly and may include:
- Severe hypotension (low blood pressure)
- Tachycardia (rapid heart rate)
- Shortness of breath or respiratory distress
- Cold, clammy skin
- Decreased urine output
- Altered mental state (confusion, anxiety, or unconsciousness)
- Neck vein distension (in cardiac tamponade or tension pneumothorax)
- Chest pain or discomfort (in pulmonary embolism or aortic dissection)
- Weak or absent pulses
The specific symptoms may vary depending on the underlying cause of the obstruction.
Causes
Obstructive shock results from conditions that impede the heart’s ability to fill or eject blood, such as:
- Tension Pneumothorax: Air trapped in the pleural space compresses the heart and great vessels.
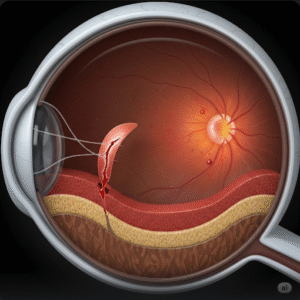
- Cardiac Tamponade: Fluid accumulation in the pericardial sac prevents the heart from expanding properly.
- Massive Pulmonary Embolism: A large blood clot in the pulmonary artery blocks blood flow from the heart to the lungs.
- Aortic Dissection: A tear in the aorta can obstruct blood flow to vital organs.
- Mediastinal masses or tumors: Compress major vessels or the heart.
- Abdominal compartment syndrome: Increased abdominal pressure compresses major vessels, impeding venous return.
Each of these conditions blocks blood flow either into or out of the heart, reducing perfusion throughout the body.
Risk Factors
Certain individuals may have a higher risk of developing obstructive shock due to:
- Severe trauma or chest injury
- Recent surgery, especially cardiac or thoracic
- Blood clotting disorders or deep vein thrombosis (DVT)
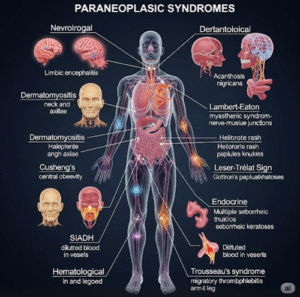
- Cancer or mediastinal tumors
- Autoimmune diseases affecting the heart or lungs
- Prolonged immobility
- Invasive procedures (e.g., central line placement)
Prompt identification of risk factors is key for prevention and rapid diagnosis.
Complications
If not recognized and treated immediately, obstructive shock can lead to:
- Multi-organ failure
- Cardiac arrest
- Severe hypoxia and acidosis
- Neurological damage
- Death
Even after successful resuscitation, long-term complications such as renal failure, lung damage, or persistent hypotension may occur depending on the duration of shock.
Prevention
Prevention depends on early identification and management of the underlying conditions:
- Prevent deep vein thrombosis (DVT) with anticoagulation in high-risk patients
- Use ultrasound guidance for central line placement to avoid cardiac tamponade
- Monitor trauma patients closely for signs of tension pneumothorax
- Post-operative monitoring in high-risk surgeries (cardiac, vascular, thoracic)
- Education and early imaging for patients with chest pain or sudden collapse
In emergency settings, rapid diagnosis and treatment protocols are critical.
Treatment Options in Korea
South Korea has highly advanced emergency medicine and critical care systems, offering world-class treatment for obstructive shock in both public and private hospitals.
1. Emergency Stabilization
- IV fluids and oxygen therapy to stabilize circulation
- Vasopressors (e.g., norepinephrine) if fluids alone are insufficient
- Advanced monitoring in the intensive care unit (ICU)
2. Definitive Treatment (Cause-Specific)
- Tension pneumothorax: Immediate needle decompression, followed by chest tube insertion
- Cardiac tamponade: Pericardiocentesis (drainage of pericardial fluid)
- Massive pulmonary embolism:
- Thrombolytic therapy
- Catheter-directed clot removal
- Surgical embolectomy in life-threatening cases
- Aortic dissection: Emergency vascular surgery or endovascular stenting
- Tumor or mass: Oncology evaluation and potential surgical resection or radiation
- Abdominal compartment syndrome: Surgical decompression
3. Critical Care Management
- Admission to ICU for close hemodynamic monitoring
- Mechanical ventilation if respiratory failure is present
- Renal support (dialysis) for kidney involvement
- Inotropic support for persistent low cardiac output
4. Top Hospitals for Emergency and Cardiac Care in Korea
- Asan Medical Center – Advanced Trauma and Cardiology Units
- Samsung Medical Center – Emergency Critical Care and Pulmonology
- Seoul National University Hospital – Cardiothoracic Surgery and Shock Unit
- Severance Hospital (Yonsei University) – Emergency and Chest Surgery
- National Medical Center – High-volume emergency care
These centers are equipped with:
- 24/7 emergency teams and surgical services
- Multidisciplinary teams (cardiology, pulmonology, surgery, critical care)
- Rapid imaging (CT, ultrasound, echocardiography)
- English-speaking international departments