Overview
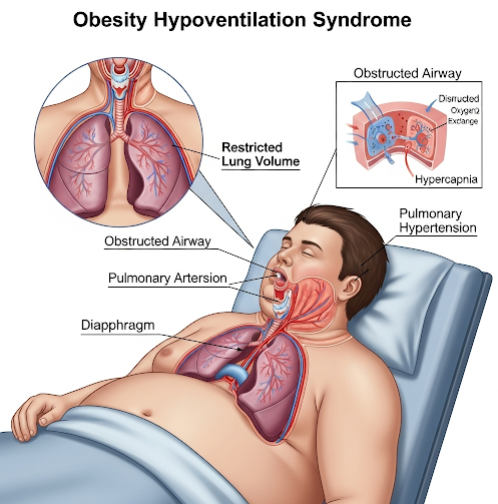
Obesity Hypoventilation Syndrome (OHS) is a serious breathing disorder that occurs in people with obesity, leading to chronic under-breathing (hypoventilation) and high carbon dioxide (CO₂) levels in the blood. It is also known as Pickwickian syndrome. OHS often coexists with obstructive sleep apnea (OSA) and causes fatigue, breathlessness, and low oxygen levels, especially during sleep.
If untreated, OHS can result in heart failure, pulmonary hypertension, and even respiratory failure. Early diagnosis and intervention can significantly improve quality of life and long-term outcomes.
What is Obesity Hypoventilation Syndrome?
OHS is defined by three key criteria:
- Obesity (BMI ≥ 30 kg/m²)
- Chronic daytime hypoventilation (elevated arterial CO₂ > 45 mmHg)
- Absence of other known causes of hypoventilation (e.g., neuromuscular disorders, lung disease)
The syndrome develops because excess fat on the chest and abdomen compresses the lungs and respiratory muscles, making it harder to breathe effectively. This leads to inadequate ventilation, particularly during sleep, causing CO₂ buildup and low oxygen levels.
Symptoms
OHS symptoms often overlap with sleep apnea, but also include features of chronic low ventilation:
- Daytime sleepiness or fatigue
- Morning headaches (due to CO₂ retention)
- Shortness of breath, especially with activity
- Snoring or choking during sleep
- Difficulty concentrating or memory problems
- Bluish skin (cyanosis) in severe cases
- Swelling in the legs (edema) due to heart strain
- Loud snoring or pauses in breathing during sleep
These symptoms often worsen over time if not treated.
Causes
OHS is primarily caused by severe obesity, which impairs the body’s ability to breathe efficiently:
- Mechanical restriction of the lungs due to excess abdominal and chest fat
- Decreased lung compliance (stiff lungs)
- Increased work of breathing
- Blunted respiratory drive from the brain due to chronic CO₂ retention
- Obstructive sleep apnea, which further reduces oxygen levels during sleep
While obesity is the main factor, genetics and environmental factors may also contribute to who develops OHS.
Risk Factors
Risk factors for developing OHS include:
- BMI ≥ 35 kg/m²
- Coexisting obstructive sleep apnea (OSA)
- Male sex (more common in men)
- Older age
- Sedentary lifestyle
- Poor respiratory muscle function
- Metabolic syndrome or insulin resistance
Not all obese individuals develop OHS, but these factors increase the likelihood.
Complications
If left untreated, OHS can lead to severe health consequences:
- Pulmonary hypertension (high blood pressure in the lungs)
- Right-sided heart failure (cor pulmonale)
- Chronic respiratory failure
- Increased risk of hospitalizations for respiratory infections
- Sudden cardiac death during sleep
- Reduced quality of life and life expectancy
Early treatment can reduce these risks significantly.
Prevention
While OHS cannot always be prevented, the best preventive strategies include:
- Weight management through a healthy diet and regular physical activity
- Screening for sleep apnea in obese individuals
- Avoiding sedatives, alcohol, or narcotics that can worsen hypoventilation
- Smoking cessation to preserve lung function
- Regular health checkups to monitor respiratory and cardiac health
For individuals already overweight or showing symptoms, early intervention is essential.
Treatment Options in Korea
South Korea provides excellent care for OHS through multidisciplinary respiratory and sleep medicine centers in major hospitals.
1. Diagnosis
- Arterial blood gas (ABG) test to measure CO₂ and O₂ levels
- Polysomnography (sleep study) to assess for sleep apnea
- Pulmonary function tests
- Chest X-ray or CT scan
- Echocardiogram to assess for heart complications
- Serum bicarbonate levels as a screening tool
2. Positive Airway Pressure (PAP) Therapy
- Noninvasive ventilation (NIV) with bilevel positive airway pressure (BiPAP)
- CPAP (Continuous Positive Airway Pressure) if OSA is dominant
- These devices support breathing during sleep and reduce CO₂ levels
3. Weight Reduction
- Calorie-controlled diet plans
- Exercise therapy under medical supervision
- Behavioral counseling for sustainable lifestyle change
- Pharmacological therapy: Anti-obesity medications (e.g., liraglutide) if appropriate
- Bariatric surgery in severe obesity (BMI ≥ 35–40) when conservative measures fail
4. Management of Comorbidities
- Treatment of hypertension, diabetes, and dyslipidemia
- Oxygen therapy in some cases (used cautiously to avoid CO₂ retention)
- Monitoring for heart and lung complications
5. Top Hospitals and Clinics in Korea
Leading institutions for OHS management include:
- Samsung Medical Center – Sleep & Respiratory Center
- Severance Hospital (Yonsei University) – Pulmonology Department
- Asan Medical Center – Sleep Disorder Clinic
- Seoul National University Hospital – Respiratory Care Center
These centers offer:
- State-of-the-art diagnostic testing
- Expert teams of pulmonologists, sleep specialists, dietitians, and surgeons
- Customized ventilation therapy programs
- Multilingual services for international patients