Overview
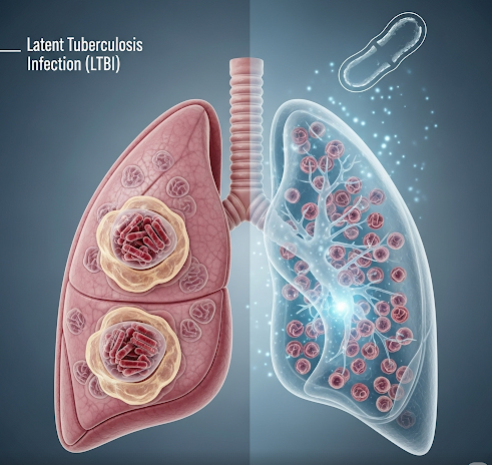
Latent Tuberculosis Infection (LTBI) occurs when a person is infected with Mycobacterium tuberculosis but does not have active disease symptoms. The bacteria remain dormant in the body without causing illness or contagiousness. However, LTBI can progress to active tuberculosis (TB) if untreated, especially in individuals with weakened immune systems.
What Is Latent Tuberculosis Infection (LTBI)?
LTBI is a condition where M. tuberculosis bacteria exist in the body in an inactive state. People with LTBI do not feel sick and cannot spread TB to others. Without treatment, about 5-10% of individuals with LTBI may develop active TB disease during their lifetime, which is contagious and symptomatic.
Symptoms
- LTBI itself causes no symptoms.
- Active TB symptoms to watch for (if progression occurs) include:
- Persistent cough lasting more than 3 weeks
- Chest pain
- Coughing up blood or sputum
- Fatigue and weakness
- Weight loss
- Fever and night sweats
Causes
- Infection by inhaling airborne droplets containing Mycobacterium tuberculosis from an active TB patient.
- LTBI occurs when the immune system contains but does not eliminate the bacteria, leading to dormant infection.
Risk Factors
- Close contact with someone with active TB
- Immunosuppressive conditions (HIV/AIDS, cancer, diabetes)
- Use of immunosuppressive drugs (steroids, chemotherapy)
- Recent infection (within 2 years) with TB
- Living or working in high TB prevalence areas
- Substance abuse (alcohol, drugs)
- Malnutrition or poor general health
Complications
- Progression from LTBI to active TB disease, which is contagious and can cause severe health issues.
- Active TB can lead to lung damage, respiratory failure, and spread to other organs if untreated.
Prevention
- Screening high-risk individuals for LTBI and offering preventive therapy.
- Avoiding close contact with active TB patients.
- Improving living conditions and ventilation in crowded places.
- Strengthening immune health through balanced nutrition and managing chronic diseases.
- Vaccination with BCG (Bacillus Calmette-Guérin) in some countries to reduce severe TB in children.
Treatment Options in Korea
Korea provides comprehensive LTBI management using internationally recommended protocols:
- Screening: TB skin test (Mantoux test) and interferon-gamma release assays (IGRA) to detect LTBI.
- Preventive Therapy: Isoniazid or rifampin-based regimens administered for several months to eliminate dormant bacteria and reduce progression risk.
- Monitoring: Regular follow-up to check for side effects and adherence to medication.
- Specialized Care: Access to pulmonologists and infectious disease specialists experienced in TB management.
- Public Health Programs: Korea’s national TB control program ensures screening, treatment, and education, helping to reduce TB burden nationwide.
With advanced diagnostic tools and effective preventive treatment, Korea offers excellent care for LTBI patients to prevent active TB and promote public health.