Overview
Kernicterus is a rare but serious form of brain damage caused by excessive accumulation of bilirubin in the brain tissue. It primarily affects newborns and infants with severe jaundice. If untreated, kernicterus can lead to permanent neurological damage, including hearing loss, movement disorders, and intellectual disabilities. Korea’s neonatal care centers are equipped with advanced screening, monitoring, and treatment protocols to prevent and manage kernicterus effectively.
What Is Kernicterus?
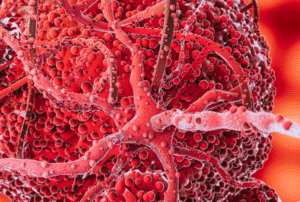
Kernicterus is a type of bilirubin-induced neurological dysfunction resulting from the toxic deposition of unconjugated bilirubin in the brain’s basal ganglia and brainstem nuclei. Bilirubin is a yellow pigment formed by the breakdown of red blood cells. Normally, bilirubin is processed by the liver and excreted, but in newborns with immature liver function or excessive breakdown of red cells, bilirubin can accumulate to dangerous levels. Kernicterus represents the most severe consequence of untreated hyperbilirubinemia (high bilirubin levels).
Symptoms
In newborns and infants, kernicterus symptoms progress through stages:
- Early signs: Poor feeding, lethargy, irritability, high-pitched crying
- Moderate signs: Muscle rigidity or floppy muscles, arching of the back (opisthotonus), seizures
- Late signs: Hearing loss, movement disorders (chorea, athetosis), developmental delay, and cognitive impairment
- Permanent symptoms may include cerebral palsy, intellectual disability, and auditory neuropathy
Causes
Kernicterus occurs due to high levels of unconjugated (indirect) bilirubin crossing the immature blood-brain barrier in newborns. Causes include:
- Hemolytic diseases such as Rh incompatibility or ABO incompatibility
- Prematurity and immature liver function
- Genetic enzyme deficiencies affecting bilirubin metabolism (e.g., G6PD deficiency)
- Excessive bruising or internal bleeding in newborns
- Infections or sepsis that impair liver function
Risk Factors
- Premature birth or low birth weight
- Blood type incompatibilities between mother and baby
- Family history of hemolytic disease or bilirubin metabolism disorders
- Delayed or inadequate treatment of neonatal jaundice
- Certain ethnic groups with higher G6PD deficiency prevalence
Complications
- Permanent neurological damage including cerebral palsy and hearing loss
- Intellectual disabilities and developmental delays
- Movement disorders such as dystonia and athetosis
- Vision and speech impairment
- Death in severe untreated cases
Prevention
- Early screening and monitoring of bilirubin levels in newborns
- Prompt treatment of neonatal jaundice with phototherapy or exchange transfusion
- Preventing hemolytic diseases through prenatal care and blood type screening
- Educating parents about recognizing jaundice signs and seeking medical care promptly
- Proper management of risk factors such as infections or prematurity
Treatment Options in Korea
Korea offers advanced neonatal care facilities specializing in early detection and treatment of hyperbilirubinemia and kernicterus prevention:
- Phototherapy: The primary treatment for reducing bilirubin levels, using special blue light to convert bilirubin into water-soluble forms that can be excreted.
- Exchange Transfusion: In severe cases, blood is replaced to rapidly remove bilirubin and antibodies causing hemolysis.
- Supportive Care: Monitoring for neurological symptoms and managing complications.
- Genetic Counseling: For families with hereditary conditions affecting bilirubin metabolism.
- Advanced Monitoring: Use of transcutaneous bilirubin meters and laboratory tests for precise bilirubin level assessment.
Korean neonatal intensive care units (NICUs) implement strict protocols to monitor at-risk newborns and provide multidisciplinary care involving neonatologists, neurologists, and audiologists to ensure early intervention and optimal outcomes.