Overview
Juvenile Nasopharyngeal Angiofibroma (JNA) is a rare, benign but highly vascular tumor that occurs almost exclusively in adolescent males. Despite being non-cancerous, it is locally aggressive and can spread into surrounding areas such as the sinuses, orbit, and even intracranial regions. In Korea, JNA is recognized as a challenging condition due to its vascularity, risk of severe bleeding, and high recurrence rate. Leading tertiary hospitals such as Seoul National University Hospital, Asan Medical Center, and Samsung Medical Center provide advanced surgical and radiological management for this rare tumor.
What is Juvenile Nasopharyngeal Angiofibroma (JNA)?
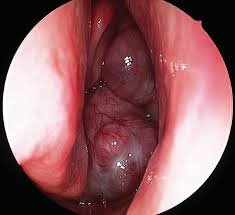
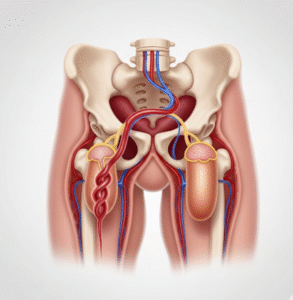
Juvenile Nasopharyngeal Angiofibroma is a benign fibrovascular tumor that originates in the nasopharynx, typically near the sphenopalatine foramen. It almost exclusively affects male adolescents between 10 and 18 years old, strongly linked to hormonal influences, particularly androgens. Although non-malignant, it can cause significant health problems because of its aggressive local growth and potential to invade nearby structures.
Symptoms
- Recurrent, often severe nosebleeds (epistaxis)
- Persistent nasal obstruction or congestion
- Facial swelling or deformity in advanced stages
- Hearing loss due to Eustachian tube blockage
- Headaches or facial pain
- Bulging eyes (proptosis) if the tumor extends into the orbit
- In rare cases, neurological symptoms when extending intracranially
Causes
The exact cause of JNA is unknown, but several factors contribute:
- Hormonal influence: Strong association with androgens explains its prevalence in adolescent males.
- Genetic predisposition: Mutations in certain Y-chromosome genes (USP9Y, UTY, DDX3Y) have been implicated in recent studies.
- Embryological origin: Believed to arise from remnants of embryonic fibrovascular tissue in the nasopharynx.
Risk Factors
- Being male (almost exclusively affects males)
- Adolescence (ages 10–18 are the peak onset years)
- Family history or genetic predisposition (rare)
- Hormonal surges during puberty
Complications
If untreated, JNA can cause:
- Chronic and severe blood loss leading to anemia
- Facial deformities due to bone invasion
- Vision problems or blindness if it spreads to the orbit
- Neurological complications when extending into the cranial cavity
- High surgical risks due to excessive intraoperative bleeding
- Recurrence even after surgery (common within the first year post-operation)
Prevention
Since JNA is largely driven by genetic and hormonal factors, there are no guaranteed preventive measures. However:
- Early detection through ENT evaluation in adolescents with recurrent nosebleeds is critical.
- Regular medical follow-up for at-risk patients can help detect tumors at an earlier, more manageable stage.
- Awareness programs in Korea encourage timely diagnosis to prevent advanced-stage complications.
Treatment Options in Korea
South Korea is highly advanced in the management of JNA, using state-of-the-art surgical and interventional techniques:
- Diagnosis
- CT and MRI scans are routinely used to define tumor extent.
- Angiography is performed to identify feeding vessels.
- Biopsy is avoided due to the risk of massive bleeding.
- Preoperative Embolization
- Commonly performed in Korean hospitals to block the blood supply to the tumor, significantly reducing surgical bleeding.
- Surgical Treatments
- Endoscopic resection: Increasingly used for stage II tumors with limited spread. Korean centers report good outcomes with lower recurrence rates in early stages.
- Open approaches (midfacial degloving, maxillary swing): Used for advanced-stage tumors. Korean studies show that the maxillary swing approach achieves better tumor control in large or complex cases.
- Combined approaches: In complex JNA, endoscopic surgery may be combined with external approaches for complete resection.
- Radiation & Radiosurgery
- For residual or recurrent tumors, Gamma Knife Radiosurgery (GKS) is available in Korea. Seoul National University Hospital successfully treated recurrent orbital JNA using GKS, achieving tumor shrinkage without complications.
- Follow-Up Care
- Patients undergo regular MRI/CT imaging within the first year after surgery to monitor for recurrence.
- Long-term ENT and neurosurgical follow-up is essential.