Overview
Itchy skin at night, medically termed nocturnal pruritus, is a widespread and often distressing symptom that affects people of all ages worldwide, including Korea. This phenomenon involves an uncomfortable urge to scratch that worsens or primarily occurs during nighttime hours, disrupting sleep and reducing quality of life. While mild itching can be a transient and benign issue, persistent or intense nocturnal itching may be a sign of underlying dermatological disorders, systemic diseases, neurological conditions, or psychological factors. The interplay of physiological and environmental influences makes nocturnal pruritus a complex symptom requiring a thorough approach for diagnosis and treatment.
In Korea, the seasonal variations—with hot, humid summers and cold, dry winters—alongside urban lifestyles contribute to increased incidences of skin dryness and related itching. Additionally, growing awareness of chronic conditions like kidney and liver diseases, which can manifest with nocturnal itching, has led to improved detection and treatment protocols. Integrative healthcare options, combining Western medicine with traditional Korean medicine such as acupuncture and herbal therapies, also provide patients with diverse options for relief.
What is Itchy Skin at Night?
Nocturnal pruritus refers specifically to itching sensations that intensify or appear predominantly at night. Several factors may explain this nocturnal pattern:
- Circadian rhythm: Histamine and other inflammatory mediators that trigger itching have natural fluctuations in the body, often peaking at night.
- Reduced external distractions: At night, fewer sensory inputs mean individuals focus more on internal sensations like itching.
- Skin physiology: At night, skin temperature rises slightly, and the skin’s barrier function can change, increasing susceptibility to dryness and irritation.
- Psychological factors: Fatigue and stress accumulation over the day can heighten perception of itch.
This symptom is not a disease itself but a manifestation that may stem from various causes, often making diagnosis challenging without detailed clinical evaluation.
Symptoms
People experiencing itchy skin at night report:
- Persistent or intermittent itching: Often localized to specific areas such as the legs, arms, or scalp but may be generalized.
- Scratching-related skin changes: Excoriations, redness, crusting, and thickened skin from chronic scratching.
- Worsening during the evening or night: Patients may notice that itching intensifies just before bedtime or after falling asleep.
- Sleep disturbances: Difficulty falling asleep, frequent awakenings, or poor sleep quality due to itching discomfort.
- Associated sensations: Burning, stinging, or crawling sensations may accompany itching, particularly in neuropathic causes.
- Secondary infections: Open sores or lesions from scratching can become infected, causing further discomfort.
Causes
Nocturnal itching arises from a broad spectrum of potential causes categorized mainly into dermatological, systemic, neurological, psychological, and environmental factors.
Dermatological Causes
- Atopic dermatitis: Characterized by dry, itchy, inflamed skin; itching typically worsens at night due to skin dryness and increased histamine.
- Psoriasis: Chronic autoimmune skin disease with scaly plaques that can itch intensely, especially at night.
- Contact dermatitis: Allergic or irritant reactions to substances such as soaps, detergents, or fabrics.
- Xerosis (dry skin): Particularly common among elderly or in winter months with low humidity, leading to tight, itchy skin.
- Scabies: Infestation by Sarcoptes scabiei mites, causing severe itching that is notably worse at night.
- Lichen simplex chronicus: Thickened skin patches from chronic scratching or rubbing, often exacerbating nocturnal itch.
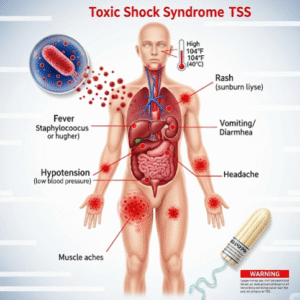
Systemic Causes
- Chronic kidney disease (CKD): Uremic pruritus affects many patients on dialysis due to toxin accumulation and altered skin metabolism.
- Liver diseases: Conditions like cholestasis cause bile salt buildup, provoking intense itching, often generalized and worse at night.
- Thyroid disorders: Hyperthyroidism can cause dry skin and itching.
- Hematologic diseases: Iron deficiency anemia, polycythemia vera, and lymphoma can present with pruritus.
- Diabetes mellitus: Peripheral neuropathy and dry skin contribute to nocturnal itching.
Neurological Causes
- Neuropathic itch: Damage or dysfunction of peripheral or central nervous system pathways, seen in multiple sclerosis, postherpetic neuralgia, or spinal cord injuries.
- Nerve entrapment or irritation: Compression syndromes can manifest as localized itching.
Psychological Causes
- Stress, anxiety, and depression: These conditions can amplify the perception of itch or cause psychogenic pruritus.
- Somatoform disorders: Itching with no identifiable organic cause.
Environmental and Lifestyle Factors
- Heat and sweating: Increased warmth and moisture at night promote skin irritation.
- Use of harsh soaps, detergents, or fragranced products.
- Exposure to allergens in bedding or clothing.
- Low humidity during cold seasons leading to skin dryness.
- Medications: Opioids, ACE inhibitors, and some diuretics can induce pruritus.
Risk Factors
- Preexisting skin conditions such as eczema or psoriasis.
- Chronic systemic illnesses like kidney or liver disease.
- Aging, due to natural decline in skin moisture and elasticity.
- Occupation or lifestyle exposures to irritants or allergens.
- Psychological stress and mental health disorders.
- Environmental exposure to dry or hot climates.
- Certain medications causing itch as a side effect.
Complications
- Sleep deprivation: Poor sleep quality leads to daytime fatigue, impaired concentration, and reduced productivity.
- Secondary skin infections: Scratching breaks the skin barrier, allowing bacteria or fungi to invade.
- Chronic skin changes: Lichenification and hyperpigmentation from repeated scratching.
- Psychological impact: Persistent itch and sleep loss contribute to anxiety, depression, and reduced quality of life.
- Social withdrawal: Embarrassment or frustration may limit social and work activities.
Prevention
- Skin care: Regular application of moisturizers to maintain skin hydration, avoiding hot baths or harsh soaps.
- Environmental control: Maintaining moderate room temperature and humidity, using air humidifiers in dry seasons.
- Avoidance of irritants: Choosing fragrance-free, gentle detergents and fabrics.
- Stress management: Incorporating relaxation techniques, physical exercise, and counseling as needed.
- Medical management: Early treatment of underlying conditions like eczema, kidney, or liver diseases.
- Bedtime routine: Wearing loose, breathable clothing and keeping bedroom cool to minimize sweating.
Treatment Options in Korea
Korean healthcare provides a multi-faceted approach for managing nocturnal itching:
- Diagnostic work-up: Comprehensive clinical evaluation with laboratory tests (liver/kidney function, blood counts, thyroid hormones), skin biopsies if needed, and allergy testing.
- Topical therapies: Prescription moisturizers, corticosteroids, and calcineurin inhibitors to reduce skin inflammation and restore barrier function.
- Systemic medications:
- Antihistamines, particularly sedating types (e.g., hydroxyzine, doxepin), to reduce itch intensity and improve sleep.
- Treatment of systemic diseases contributing to pruritus (e.g., ursodeoxycholic acid for cholestasis, dialysis optimization for kidney disease).
- Neuropathic agents like gabapentin or pregabalin for nerve-related itch.
- Phototherapy: Narrowband UVB phototherapy is widely available and effective for chronic inflammatory skin diseases.
- Psychological support: Cognitive behavioral therapy and stress reduction programs to address itch amplification from anxiety or depression.
- Traditional Korean medicine: Acupuncture and herbal medicine offer adjunctive benefits by modulating immune response and improving circulation.
- Patient education: On skincare, environmental modifications, and avoidance of triggers.
- Follow-up: Regular monitoring for treatment efficacy and side effects.