Overview
Ischemic colitis is a common form of intestinal ischemia resulting from reduced or interrupted blood flow to the colon. This decrease in perfusion causes inflammation, injury, and in severe cases, necrosis (tissue death) of the colonic mucosa. Ischemic colitis mainly affects the elderly population and those with underlying vascular or cardiac diseases but can occur at any age. The severity of the condition ranges from mild, self-limiting inflammation that resolves with supportive care to fulminant ischemia requiring emergency surgery. It represents a significant cause of abdominal pain and lower gastrointestinal bleeding, making early diagnosis and treatment essential to prevent complications. In Korea, with its aging population and rising vascular disease incidence, ischemic colitis is an important clinical problem managed with advanced diagnostic and therapeutic protocols.
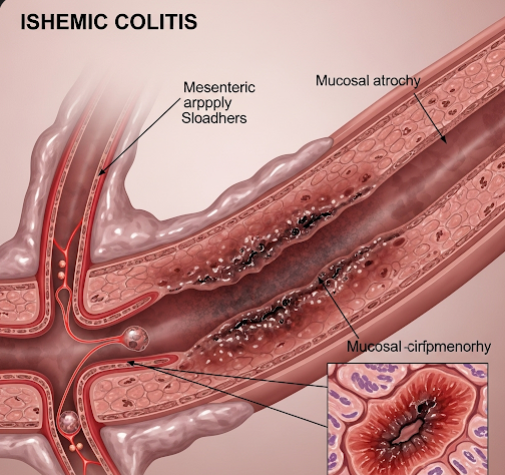
What is Ischemic Colitis?
Ischemic colitis is inflammation and injury of the colon caused by insufficient blood flow, primarily due to impaired perfusion through the mesenteric arteries or their branches. The colon has a rich but vulnerable blood supply from the superior and inferior mesenteric arteries, with watershed areas (regions between arterial territories) like the splenic flexure and sigmoid colon being especially susceptible to ischemia.
When the blood supply drops below a critical threshold, colonic tissues become oxygen-starved. This hypoxia causes:
- Breakdown of the mucosal barrier.
- Cellular injury and death.
- Inflammatory response with edema and ulceration.
- If prolonged, transmural infarction and perforation.
Unlike ischemia in other organs, the colon often manifests with bloody diarrhea and crampy abdominal pain, highlighting the mucosal involvement.
Symptoms
Ischemic colitis symptoms often begin suddenly and include:
- Abdominal pain: Typically cramping and localized to the left lower quadrant or mid-abdomen. The pain is often severe but may be intermittent.
- Urgent bowel movements: Frequent defecation urges often accompany the pain.
- Bloody diarrhea or passage of bloody mucus: Due to mucosal ulceration and bleeding.
- Abdominal tenderness: On physical examination, localized tenderness without peritoneal signs in mild cases.
- Nausea and vomiting: More common in severe or extensive ischemia.
- Fever: Usually low-grade but can rise in complicated cases.
- Signs of systemic illness: Hypotension, tachycardia, and signs of sepsis in severe ischemia or perforation.
Symptoms can range from mild and self-limited to severe with signs of acute abdomen requiring emergent care.
Causes
Ischemic colitis develops due to a variety of mechanisms that impair blood flow to the colon:
- Atherosclerosis: Chronic narrowing of mesenteric arteries due to plaque buildup is the most common cause, especially in elderly patients.
- Systemic hypotension: From heart failure, shock, dehydration, or blood loss leading to low perfusion pressure.
- Embolic or thrombotic occlusion: Blood clots or emboli lodging in mesenteric arteries.
- Vasculitis: Autoimmune or inflammatory conditions such as systemic lupus erythematosus or polyarteritis nodosa causing vessel inflammation and occlusion.
- Medications: Drugs like digitalis, vasopressors, or cocaine that induce vasoconstriction can precipitate ischemia.
- Surgical procedures or trauma: Injury to mesenteric vessels during abdominal operations or blunt trauma.
- Mechanical factors: Volvulus, hernias, or strictures causing vessel compression.
- Hypovolemia: Severe dehydration or hemorrhage reducing circulating volume.
Risk Factors
Individuals at increased risk include:
- Age: Most cases occur in patients over 60 years.
- Cardiovascular disease: Including coronary artery disease, heart failure, arrhythmias (especially atrial fibrillation).
- Peripheral artery disease or previous stroke.
- Diabetes mellitus: Contributing to microvascular disease.
- Smoking: Accelerates atherosclerosis.
- Use of certain medications: Especially vasoconstrictive agents.
- Recent major surgery or critical illness.
- Dehydration or volume depletion.
- Hypercoagulable states: Increasing thrombosis risk.
Complications
Without timely intervention, ischemic colitis can lead to severe consequences:
- Full-thickness colonic infarction: Leading to necrosis and loss of bowel viability.
- Colonic perforation: Leakage of bowel contents causing peritonitis, a surgical emergency.
- Sepsis and multi-organ failure: From systemic infection secondary to bowel perforation.
- Strictures and chronic ischemic colitis: Long-term scarring leading to bowel obstruction or chronic diarrhea.
- Persistent bleeding: Leading to anemia.
- Recurrence: Especially if underlying risk factors remain uncontrolled.
Prevention
Preventive strategies focus on managing risk factors and maintaining vascular health:
- Control cardiovascular risk factors: Aggressive management of hypertension, diabetes, hyperlipidemia.
- Smoking cessation: To reduce vascular injury and atherosclerosis progression.
- Maintain adequate hydration: Especially in elderly or critically ill patients.
- Avoid or cautiously use vasoconstrictive medications.
- Early recognition and management of atrial fibrillation: To prevent embolic events.
- Regular monitoring and treatment of peripheral artery disease.
- Prompt treatment of acute hypotension and shock states.
Treatment Options in Korea
In Korea, ischemic colitis is managed through a multidisciplinary approach combining gastroenterology, surgery, and critical care teams:
- Diagnosis:
- Colonoscopy: The gold standard for diagnosis, revealing pale mucosa with petechial hemorrhages, edema, ulcerations, and segmental involvement. Biopsies help rule out infectious or inflammatory colitis.
- Contrast-enhanced abdominal CT scan: Identifies bowel wall thickening, pneumatosis (air in bowel wall), portal venous gas, or signs of perforation.
- Blood tests: Elevated white blood cells, lactic acid, and inflammatory markers.
- Mesenteric angiography: In select cases to assess arterial patency or for interventional therapy.
- Medical management:
- Supportive care with bowel rest (nothing by mouth), intravenous fluids, and electrolyte correction.
- Pain management with cautious use of analgesics.
- Monitoring and treatment of underlying causes such as heart failure or arrhythmias.
- Broad-spectrum antibiotics if infection or bowel necrosis is suspected.
- Avoidance of unnecessary surgical interventions in mild cases, as many recover with conservative care.
- Surgical treatment:
- Indicated in patients with bowel necrosis, perforation, peritonitis, or worsening clinical status despite medical therapy.
- Surgery involves resection of necrotic bowel segments with or without temporary colostomy or ileostomy.
- Postoperative care includes intensive monitoring and rehabilitation.
- Follow-up care:
- Colonoscopy to assess mucosal healing and detect strictures.
- Long-term management of cardiovascular risk factors.
- Nutritional support and counseling to prevent recurrence.
- Advanced therapies:
- In cases of embolic causes, anticoagulation or interventional radiology procedures may be applied to restore blood flow.
- Korea’s high-volume tertiary hospitals offer expertise in minimally invasive surgery and endovascular treatments improving patient outcomes.