Overview
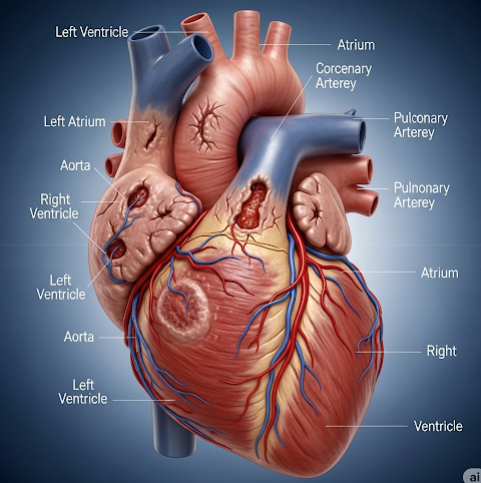
Ischemic cardiomyopathy (ICM) is a chronic and progressive heart muscle disease resulting from prolonged inadequate blood supply to the myocardium (heart muscle) caused primarily by coronary artery disease (CAD). This persistent ischemia leads to myocardial injury, scarring (fibrosis), and loss of contractile function, especially in the left ventricle, the heart’s main pumping chamber. The damaged heart muscle weakens, dilates, and becomes inefficient at pumping blood, which ultimately causes heart failure symptoms and increases morbidity and mortality risk. In Korea, ICM is a leading cause of heart failure admissions, reflecting the rising prevalence of cardiovascular diseases due to aging populations and lifestyle factors. The country’s advanced cardiovascular care infrastructure, including early diagnostic imaging, interventional cardiology, surgical techniques, and multidisciplinary management, significantly improves outcomes for ICM patients.
What is Ischemic Cardiomyopathy?
Ischemic cardiomyopathy is defined as left ventricular systolic dysfunction and heart failure that occur as a direct consequence of ischemic heart disease. It results when coronary artery obstructions reduce blood flow enough to cause repeated or chronic myocardial ischemia, infarction, or hibernation of heart muscle cells. Unlike other cardiomyopathies, ischemic cardiomyopathy has a distinct etiology tied to atherosclerosis-driven coronary artery narrowing and subsequent myocardial damage.
The heart muscle responds to ischemia by remodeling itself structurally and functionally:
- Myocyte death: Persistent oxygen deprivation causes irreversible loss of heart muscle cells replaced by fibrous scar tissue.
- Left ventricular dilation: The ventricle enlarges to compensate for reduced contractile force but this leads to inefficient pumping and increased wall stress.
- Neurohormonal activation: Compensatory mechanisms like activation of the renin-angiotensin-aldosterone system (RAAS) and sympathetic nervous system worsen remodeling and heart failure progression.
- Electrical remodeling: Increases susceptibility to arrhythmias and sudden cardiac death.
Symptoms
Ischemic cardiomyopathy presents with a spectrum of symptoms reflecting progressive heart failure and ongoing ischemia:
- Exertional dyspnea: Shortness of breath during physical activity is an early symptom due to decreased cardiac output and pulmonary congestion.
- Orthopnea and paroxysmal nocturnal dyspnea: Difficulty breathing when lying flat or sudden nighttime breathlessness due to fluid accumulation in lungs.
- Fatigue and exercise intolerance: Poor perfusion of muscles leads to tiredness and inability to sustain normal activities.
- Chest pain or angina: Recurring ischemic episodes cause discomfort or tightness, often precipitated by exertion or stress.
- Peripheral edema: Swelling of lower limbs and abdomen from fluid retention and venous congestion.
- Palpitations or syncope: Irregular heartbeats or fainting spells may indicate arrhythmias.
- Cough, wheezing, or frothy sputum: Signs of pulmonary edema in advanced cases.
- Weight gain: From fluid overload.
- Confusion or cognitive decline: Due to poor cerebral perfusion in severe heart failure.
Causes
The underlying cause of ischemic cardiomyopathy is coronary artery disease leading to myocardial ischemia and infarction:
- Atherosclerosis: Progressive plaque accumulation in coronary arteries narrows lumen size, restricting oxygen-rich blood delivery.
- Acute coronary events: Thrombosis over ruptured plaques cause myocardial infarction, killing heart muscle cells.
- Repeated ischemic insults: Chronic insufficient perfusion damages myocardium even without infarction (hibernating myocardium).
- Microvascular dysfunction: Small vessel disease further impairs myocardial blood flow, common in diabetics.
- Coronary artery spasm: Transient vessel constriction can worsen ischemia.
- Collateral circulation inadequacy: Failure to develop alternative blood supply routes worsens ischemic damage.
Risk Factors
- Non-modifiable:
- Age (risk increases after 45 years in men, 55 in women)
- Male gender
- Family history of premature CAD
- Modifiable:
- Smoking
- Hypertension
- Diabetes mellitus
- Hyperlipidemia (high LDL cholesterol)
- Obesity and metabolic syndrome
- Sedentary lifestyle
- Poor diet high in saturated fats and sugars
- Chronic stress
- Other:
- Chronic kidney disease
- Previous myocardial infarction or unstable angina
- Inflammatory diseases (e.g., rheumatoid arthritis)
Complications
Ischemic cardiomyopathy can lead to multiple serious complications:
- Chronic heart failure: Progressive pump failure causes fluid buildup in lungs and systemic circulation.
- Life-threatening arrhythmias: Ventricular tachycardia and fibrillation increase risk of sudden cardiac death.
- Thromboembolic events: Poor ventricular contraction causes blood stasis and clot formation, potentially leading to stroke or systemic embolism.
- Mitral regurgitation: Ventricular dilation distorts mitral valve function, worsening heart failure.
- Cardiogenic shock: Severe pump failure causes inadequate perfusion of vital organs.
- Multi-organ dysfunction: Resulting from chronic hypoperfusion and congestion.
Prevention
Primary and secondary prevention strategies are essential to reduce the burden of ischemic cardiomyopathy:
- Lifestyle modifications: Smoking cessation, regular exercise, balanced diet, weight management.
- Control of cardiovascular risk factors: Aggressive management of hypertension, diabetes, and hyperlipidemia.
- Medications: Use of statins, antiplatelet agents, and antihypertensives as appropriate.
- Early detection: Routine screening for coronary artery disease and prompt treatment of angina or myocardial infarction.
- Patient education: Awareness of symptom recognition and adherence to treatment plans.
Treatment Options in Korea
Korea is recognized for its sophisticated cardiovascular care, with treatment of ischemic cardiomyopathy encompassing multiple modalities:
- Diagnostic evaluations:
- Electrocardiography (ECG): Identifies ischemic changes and arrhythmias.
- Echocardiography: Assesses left ventricular size, function, and valvular involvement.
- Coronary angiography: Visualizes extent and location of coronary artery disease.
- Cardiac MRI: Provides detailed tissue characterization and viability assessment.
- Stress tests: Evaluate inducible ischemia and functional capacity.
- Medical management:
- Anti-ischemic agents: Beta-blockers reduce heart rate and oxygen demand; nitrates relieve angina; calcium channel blockers aid vasodilation.
- Heart failure medications: ACE inhibitors or ARBs prevent remodeling; mineralocorticoid receptor antagonists reduce fluid overload; diuretics manage congestion.
- Antithrombotic therapy: Aspirin or other antiplatelet agents prevent clot formation.
- Statins: Lower cholesterol and stabilize plaques.
- Novel agents: Ivabradine and angiotensin receptor-neprilysin inhibitors (ARNIs) have improved outcomes.
- Revascularization therapies:
- Percutaneous coronary intervention (PCI): Balloon angioplasty and stent placement to restore blood flow.
- Coronary artery bypass grafting (CABG): Surgical revascularization for multi-vessel disease or complex lesions.
- Hybrid procedures: Combining PCI and surgery for optimal outcomes.
- Device therapy:
- Implantable cardioverter-defibrillators (ICDs): Prevent sudden cardiac death in patients with low ejection fraction.
- Cardiac resynchronization therapy (CRT): Biventricular pacing improves ventricular coordination and function in select patients.
- Advanced therapies:
- Mechanical circulatory support: Ventricular assist devices as bridge to transplant or destination therapy.
- Heart transplantation: Considered in end-stage refractory disease.
- Rehabilitation and support:
- Structured cardiac rehabilitation programs improve exercise tolerance and quality of life.
- Nutritional counseling and psychosocial support enhance adherence.
- Research and innovation: Korea is actively involved in clinical trials investigating regenerative therapies, novel pharmacological agents, and personalized medicine approaches to improve ischemic cardiomyopathy outcomes.