Overview
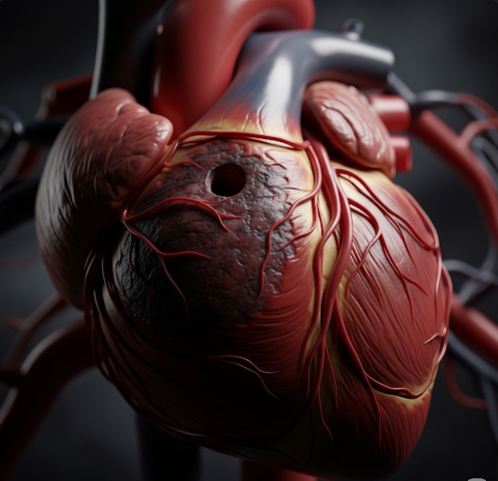
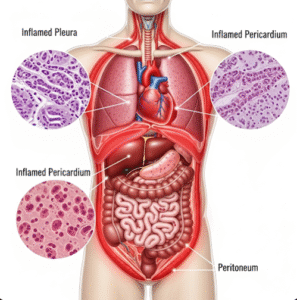
Ischemia is a pathological condition characterized by the reduction or complete obstruction of blood flow to tissues or organs, leading to a deficiency in oxygen and essential nutrients necessary for cellular metabolism and survival. This compromised blood supply can cause reversible tissue dysfunction initially but, if prolonged, may result in irreversible damage and necrosis (cell death). Ischemia can affect various organs, including the heart (myocardial ischemia), brain (cerebral ischemia), limbs (peripheral ischemia), kidneys, intestines, and other tissues. In Korea, the burden of ischemic diseases remains significant, but advances in medical technology, preventive care, and specialized treatment have greatly improved patient outcomes.
What is Ischemia?
Ischemia refers to an inadequate blood supply caused by obstruction or narrowing of blood vessels, typically arteries. The lack of sufficient blood flow limits oxygen (hypoxia) and nutrient delivery while impairing waste removal from tissues. The severity of ischemia depends on:
- The extent and speed of blood flow reduction.
- The presence of collateral circulation (alternative blood routes).
- The metabolic demands of the affected tissue.
- The duration of ischemic insult.
Ischemia may be transient or chronic and can lead to infarction (tissue death) if blood flow is not restored promptly.
Symptoms
Symptoms of ischemia vary widely depending on the organ involved and the degree of blood flow impairment:
- Myocardial ischemia (heart):
- Angina pectoris — chest pain or pressure, often radiating to the arm, neck, or jaw.
- Dyspnea (shortness of breath).
- Fatigue and palpitations.
- In severe cases, myocardial infarction (heart attack) with prolonged chest pain and other systemic symptoms.
- Cerebral ischemia (brain):
- Sudden weakness or numbness, especially on one side of the body.
- Speech difficulties (aphasia or dysarthria).
- Visual disturbances or sudden loss of vision.
- Dizziness, loss of balance, or coordination problems.
- Transient ischemic attacks (TIAs) presenting as brief neurological deficits.
- Stroke causing permanent neurological damage if ischemia persists.
- Peripheral ischemia (limbs):
- Claudication — pain in legs or arms during exercise due to inadequate blood flow.
- Cold, pale, or bluish skin.
- Weak or absent pulses distal to the blockage.
- Ulcers or gangrene in severe cases.
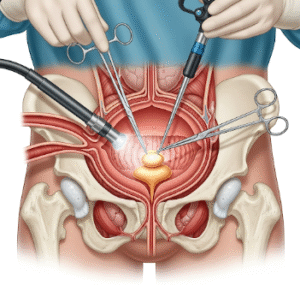
- Intestinal ischemia:
- Sudden, severe abdominal pain out of proportion to physical findings.
- Nausea and vomiting.
- Bloody diarrhea or passage of bloody stools.
- Signs of sepsis in advanced stages.
- Other organs: Symptoms depend on the affected site and may include kidney dysfunction, limb numbness, or pain.
Causes
Ischemia results primarily from obstruction or narrowing of blood vessels, with the main causes including:
- Atherosclerosis: Accumulation of lipid plaques causing progressive arterial narrowing and reduced lumen diameter.
- Thrombosis: Formation of blood clots within vessels, obstructing blood flow.
- Embolism: Dislodged clots, fat, air, or tumor fragments traveling and occluding distant vessels.
- Vasospasm: Sudden constriction of arteries (e.g., coronary artery spasm).
- External compression: Trauma, tumors, or compartment syndromes compressing vessels.
- Low perfusion states: Severe hypotension, shock, or cardiac arrest reducing overall blood flow.
- Inflammatory diseases: Vasculitis causing vessel wall inflammation and narrowing.
- Congenital anomalies: Rare structural vascular defects.
Risk Factors
Several factors increase susceptibility to ischemia:
- Lifestyle: Smoking, physical inactivity, unhealthy diet.
- Chronic conditions: Hypertension, diabetes mellitus, dyslipidemia (high cholesterol).
- Age: Risk increases with advancing age.
- Family history: Genetic predisposition to cardiovascular diseases.
- Obesity: Contributes to metabolic syndrome.
- Stress: Chronic stress can exacerbate vascular conditions.
- Other: Previous ischemic events, atrial fibrillation, coagulation disorders.
Complications
If ischemia is not promptly recognized and treated, it can lead to serious complications:
- Tissue infarction: Permanent death of tissue resulting in loss of function.
- Organ failure: Heart failure, stroke-related disabilities, kidney failure, or limb loss.
- Arrhythmias: Irregular heart rhythms caused by myocardial ischemia.
- Chronic pain: Especially in peripheral arterial disease.
- Infection and sepsis: From tissue necrosis or ulceration.
- Psychosocial impact: Disability, reduced quality of life, emotional distress.
Prevention
Preventing ischemia focuses largely on controlling risk factors and promoting cardiovascular health:
- Healthy lifestyle: Balanced diet rich in fruits, vegetables, whole grains, and low in saturated fats and salt.
- Regular physical activity: At least 150 minutes of moderate exercise per week.
- Smoking cessation: To reduce vascular damage and improve circulation.
- Blood pressure control: Maintaining optimal levels to prevent vessel damage.
- Diabetes management: Tight glucose control to reduce vascular complications.
- Cholesterol lowering: Use of statins and other lipid-lowering agents as needed.
- Weight management: Maintaining a healthy body weight.
- Regular medical check-ups: Early detection and treatment of cardiovascular risks.
- Medication adherence: For those with existing cardiovascular or metabolic conditions.
Treatment Options in Korea
Korea offers advanced medical and surgical treatments for ischemic conditions, often through multidisciplinary teams in specialized centers:
- Diagnostic modalities:
- Electrocardiogram (ECG) and stress tests for myocardial ischemia.
- Cerebral imaging (MRI, CT, angiography) for cerebral ischemia and stroke evaluation.
- Doppler ultrasound and ankle-brachial index for peripheral arterial disease.
- CT angiography or conventional angiography to visualize vascular obstructions.
- Laboratory tests for cardiac biomarkers, coagulation profiles, and lipid panels.
- Medical management:
- Antiplatelet therapy: Aspirin, clopidogrel to prevent clot formation.
- Anticoagulants: Warfarin, direct oral anticoagulants for embolism prevention.
- Thrombolytic therapy: Clot-busting drugs for acute stroke or myocardial infarction.
- Vasodilators: Nitrates, calcium channel blockers to improve blood flow.
- Statins: To stabilize atherosclerotic plaques and reduce cholesterol.
- Blood pressure and diabetes control medications.
- Interventional procedures:
- Percutaneous coronary intervention (angioplasty with stent placement).
- Carotid artery stenting.
- Peripheral angioplasty and stenting.
- Thrombectomy for stroke.
- Bypass surgery (coronary artery bypass grafting, peripheral bypass).
- Rehabilitation:
- Cardiac rehabilitation programs to improve cardiovascular health post-event.
- Physical therapy for stroke and limb ischemia recovery.
- Lifestyle modification support and counseling.
- Emerging therapies:
- Stem cell and regenerative medicine approaches under research.
- Advanced imaging and monitoring technologies.