Overview
Isaacs’ Syndrome, also called acquired neuromyotonia, is a rare autoimmune neuromuscular disorder characterized by continuous, involuntary muscle activity caused by peripheral nerve hyperexcitability. It leads to muscle stiffness, cramping, fasciculations (visible muscle twitching), and delayed muscle relaxation. This persistent abnormal muscle activity occurs because the nerves that control muscles become overactive due to an autoimmune attack on voltage-gated potassium channels (VGKC) in the nerve membranes. Isaacs’ Syndrome can severely affect quality of life with chronic symptoms and may be associated with other autoimmune diseases or tumors. In Korea, neurologists employ advanced diagnostic testing and immunotherapy to provide personalized care that helps control symptoms and improve function.
What is Isaacs’ Syndrome?
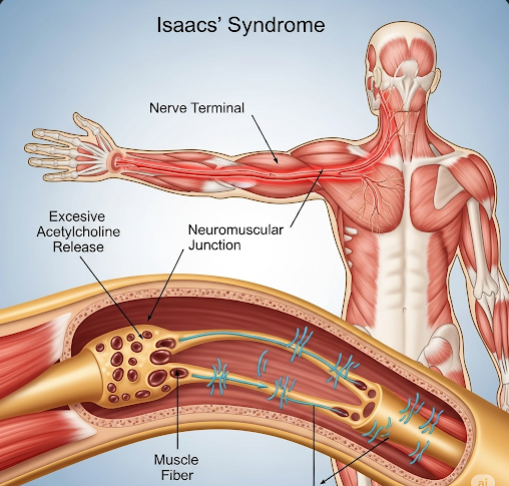
Isaacs’ Syndrome is a peripheral nerve disorder marked by continuous, spontaneous muscle fiber activity at rest, reflecting nerve hyperexcitability. Normally, potassium channels on nerve cells regulate the electrical signals that control muscle contraction by repolarizing nerve membranes after firing. In Isaacs’ Syndrome, autoantibodies target these voltage-gated potassium channels, disrupting their function and causing persistent nerve firing.
This leads to continuous muscle contractions, even when the muscles are supposed to be relaxed. The condition manifests with muscle stiffness, cramps, twitching, and myokymia (rippling of muscles under the skin). It differs from other neuromuscular disorders because the muscle activity is ongoing and not triggered solely by voluntary movement or external stimuli.
Isaacs’ Syndrome may be idiopathic or associated with underlying systemic autoimmune diseases, malignancies (paraneoplastic syndromes), or infections.
Symptoms
The clinical presentation of Isaacs’ Syndrome can vary but typically includes:
- Muscle stiffness and cramps: Persistent and often painful contractions affecting limbs, trunk, and face.
- Fasciculations: Visible, involuntary muscle twitches beneath the skin.
- Myokymia: Continuous, rippling movements of muscle fibers.
- Delayed muscle relaxation: After voluntary contraction, patients may notice a lag before muscles fully relax.
- Muscle hypertrophy: Enlargement of muscles due to chronic activity.
- Muscle weakness or fatigue: Over time, muscle exhaustion may develop.
- Sensory symptoms: Tingling, numbness, or burning sensations, though primarily a motor disorder.
- Autonomic symptoms: Excessive sweating (hyperhidrosis), heat intolerance, or other dysautonomia signs.
- Sleep disturbances: Muscle twitching and cramps may interfere with restful sleep.
- Occasionally, weakness or atrophy: In advanced or untreated cases.
Causes
Isaacs’ Syndrome is primarily autoimmune, with the following etiologies:
- Autoantibodies against VGKC: These antibodies target the voltage-gated potassium channels on peripheral nerves, especially those involving the Kv1 subunits, disrupting nerve repolarization and causing hyperexcitability.
- Paraneoplastic syndrome: It can be associated with tumors, especially thymoma, small cell lung carcinoma, or lymphoma. The immune system’s response to tumor antigens cross-reacts with nerve components.
- Other autoimmune disorders: Isaacs’ Syndrome can coexist with conditions like myasthenia gravis, systemic lupus erythematosus, or rheumatoid arthritis.
- Idiopathic: In many cases, no underlying trigger is found.
- Infections: Rarely, viral or bacterial infections may precipitate autoimmune activity.
Risk Factors
- Age between 30 and 60 years, but can affect any age.
- Personal or family history of autoimmune diseases.
- Presence of tumors known to cause paraneoplastic syndromes.
- Genetic predisposition to immune dysregulation.
- Previous infections or immune system challenges.
Complications
- Chronic pain and discomfort: From persistent muscle cramps and stiffness.
- Functional impairment: Difficulty with activities of daily living due to muscle rigidity and fatigue.
- Sleep disruption: Leading to daytime fatigue and cognitive difficulties.
- Autonomic dysfunction: Potential cardiovascular and gastrointestinal symptoms.
- Psychological impact: Anxiety and depression due to chronic illness burden.
- Secondary muscle damage: Rarely, prolonged muscle overactivity can cause structural damage.
Prevention
Because Isaacs’ Syndrome is autoimmune, specific prevention is challenging. However:
- Early diagnosis and management of autoimmune diseases may reduce risk.
- Regular cancer screenings in at-risk individuals to detect tumors early.
- Avoidance of infections and prompt treatment of illnesses that may trigger autoimmune responses.
- Maintaining general immune health through healthy lifestyle choices.
Treatment Options in Korea
Korean neurological centers employ a multidisciplinary approach for diagnosis and treatment:
- Diagnostic Tools:
- Electromyography (EMG): Shows characteristic continuous muscle fiber activity, myokymic discharges, and neuromyotonia patterns.
- Nerve conduction studies: Assess nerve function and rule out other neuropathies.
- Serological tests: Detect antibodies against VGKC and associated proteins like LGI1 and CASPR2.
- Imaging: MRI or CT scans to identify underlying tumors (thymoma, lung cancer).
- Additional blood tests: To screen for coexisting autoimmune diseases.
- Medical Treatment:
- Immunotherapies:
- Corticosteroids to suppress autoimmune activity.
- Intravenous immunoglobulin (IVIG) for immunomodulation.
- Plasmapheresis to remove circulating autoantibodies.
- Immunosuppressants such as azathioprine or mycophenolate mofetil for long-term control.
- Symptomatic treatments:
- Anticonvulsants like carbamazepine, phenytoin, or gabapentin to reduce nerve hyperexcitability and muscle symptoms.
- Muscle relaxants to relieve stiffness and cramps.
- Analgesics for pain management.
- Treatment of associated tumors: Surgical removal or oncological therapies if paraneoplastic.
- Immunotherapies:
- Supportive Care:
- Physical therapy to maintain muscle strength and flexibility.
- Occupational therapy to assist with daily activities.
- Psychological counseling to address chronic disease stress.
- Sleep hygiene measures to improve rest.
- Follow-Up:
- Regular neurologic assessments to monitor treatment response.
- Adjustment of immunotherapy and symptomatic medications as needed.
- Surveillance for tumor recurrence or emergence of additional autoimmune disorders.