Overview
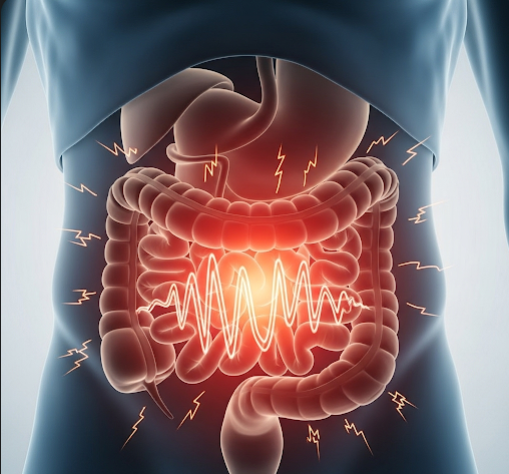
Irritable Bowel Syndrome (IBS) is a common functional gastrointestinal disorder characterized by chronic abdominal pain and altered bowel habits without any detectable structural or biochemical abnormalities. Affecting up to 10-15% of the global population, IBS significantly impacts quality of life. In Korea, awareness and management of IBS have improved with advances in gastroenterology, dietary interventions, and psychological therapies, helping patients achieve better symptom control and daily functioning.
What Is Irritable Bowel Syndrome (IBS)?
IBS is a disorder of gut-brain interaction that leads to abnormal gastrointestinal motility and heightened visceral sensitivity. It manifests as recurrent abdominal discomfort or pain associated with changes in stool frequency or form, such as diarrhea, constipation, or alternating patterns. Unlike inflammatory bowel diseases, IBS does not cause inflammation or damage to the digestive tract but can cause substantial discomfort and distress.
Symptoms
- Recurrent abdominal pain or cramping, often relieved by defecation
- Changes in bowel habits including diarrhea, constipation, or mixed patterns
- Bloating and abdominal distension
- Excessive gas and flatulence
- Mucus in the stool
- Urgency or a feeling of incomplete evacuation
- Fatigue and sleep disturbances in some cases
Causes
The exact cause of IBS remains unclear but involves multiple factors:
- Abnormal gastrointestinal motility causing irregular bowel movements
- Visceral hypersensitivity leading to increased pain perception
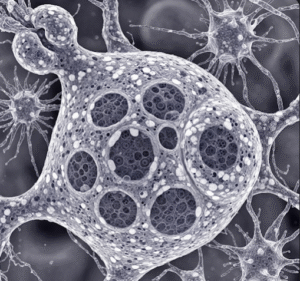
- Altered gut microbiota or dysbiosis
- Post-infectious changes following gastrointestinal infections
- Psychological stress and anxiety affecting gut-brain communication
- Food intolerances or sensitivities, such as to FODMAPs (fermentable oligo-, di-, mono-saccharides, and polyols)
Risk Factors
- Female gender, with women more commonly affected
- Younger age groups, especially under 50 years
- History of gastrointestinal infections
- Psychological conditions like anxiety and depression
- High-stress lifestyles
- Certain dietary habits including high intake of fatty or spicy foods
Complications
- Chronic discomfort and impaired quality of life
- Social withdrawal and absenteeism from work or school
- Coexisting psychological disorders such as depression or anxiety
- Nutritional deficiencies from restrictive diets
- Increased healthcare utilization without structural disease
Prevention
- Managing stress through relaxation techniques, exercise, or counseling
- Avoiding known dietary triggers and following balanced nutrition
- Maintaining regular bowel habits and hydration
- Probiotics or prebiotics to support gut microbiota balance
- Early consultation with healthcare professionals for gastrointestinal symptoms
Treatment Options in Korea
Korean healthcare offers a multidisciplinary approach to IBS management:
- Dietary Interventions:
- Low FODMAP diet supervised by nutritionists
- Identifying and avoiding individual food triggers
- Adequate fiber intake tailored to IBS subtype
- Medications:
- Antispasmodics to relieve abdominal cramps
- Laxatives or antidiarrheals depending on bowel habit
- Low-dose antidepressants to modulate pain perception and gut motility
- Probiotics to restore healthy gut flora
- Psychological Therapies:
- Cognitive-behavioral therapy (CBT) and stress management
- Mindfulness-based therapies and relaxation techniques
- Complementary Therapies:
- Traditional Korean medicine, acupuncture, and herbal treatments used adjunctively
- Patient Education:
- Comprehensive counseling on IBS nature, management strategies, and lifestyle modifications
Korea’s integrated healthcare model emphasizes personalized treatment plans combining modern medicine with complementary approaches, helping patients lead healthier, symptom-controlled lives.