Overview
Irregular periods, also known as menstrual irregularities, refer to variations in the timing, duration, and flow of menstruation that deviate from the typical menstrual cycle. The normal menstrual cycle lasts about 21 to 35 days, with bleeding lasting between 3 and 7 days. When these parameters vary significantly—such as cycles that are too frequent, too infrequent, excessively heavy, or entirely absent—it is considered irregular menstruation. This condition affects women of all ages, from adolescents experiencing the onset of menstruation to women approaching menopause. Persistent irregular periods may signal underlying health issues, hormonal imbalances, or reproductive disorders that require timely diagnosis and management. In Korea, the availability of sophisticated diagnostic tools, skilled gynecologists, and integrative treatment approaches has improved outcomes for women facing menstrual irregularities.
What is Irregular Periods?
Irregular periods encompass a wide range of menstrual cycle disturbances. They can be classified broadly as:
- Oligomenorrhea: Infrequent menstruation, with cycles longer than 35 days.
- Polymenorrhea: Frequent menstruation, with cycles shorter than 21 days.
- Amenorrhea: Absence of menstruation for three or more consecutive months.
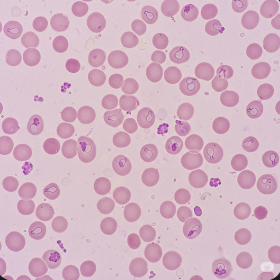
- Menorrhagia: Excessively heavy or prolonged menstrual bleeding, often leading to anemia.
- Metrorrhagia: Bleeding between periods or spotting outside the normal cycle.
These irregularities often stem from disruptions in the hypothalamic-pituitary-ovarian (HPO) axis, which regulates the menstrual cycle through hormonal feedback loops. When this axis is disrupted—due to physiological, pathological, or environmental factors—the normal rhythm of menstruation is altered.
Symptoms
Women with irregular periods may experience:
- Variability in menstrual cycle length, from very short to very long intervals.
- Changes in menstrual flow volume and duration—ranging from scanty to very heavy bleeding.
- Spotting or bleeding between cycles.
- Complete cessation of periods for extended durations.
- Associated symptoms such as pelvic or lower abdominal pain, cramping, bloating, and breast tenderness.
- Signs of anemia like fatigue, weakness, and pale complexion if bleeding is excessive.
- Mood disturbances, irritability, or depression linked to hormonal fluctuations.
- Infertility or difficulty conceiving due to irregular ovulation or anovulation.
Causes
Irregular periods have multifactorial causes. The most common include:
- Polycystic Ovary Syndrome (PCOS): A hormonal disorder causing irregular or absent ovulation, elevated androgens, and cystic ovaries. It is one of the leading causes of menstrual irregularities.
- Thyroid disorders: Both hypothyroidism and hyperthyroidism disrupt menstrual cycles by affecting the metabolism and hormone balance.
- Hyperprolactinemia: Elevated prolactin levels, often due to pituitary adenomas, can inhibit ovulation and cause amenorrhea or irregular bleeding.
- Stress and lifestyle factors: Physical or emotional stress, excessive exercise, or rapid weight loss can interfere with the HPO axis, leading to irregular cycles.
- Perimenopause: Hormonal fluctuations during the transition to menopause cause irregular cycles and changes in flow.
- Uterine abnormalities: Fibroids, polyps, adenomyosis, or endometrial hyperplasia can cause abnormal bleeding patterns.
- Medications: Hormonal contraceptives, anticoagulants, chemotherapy, or psychiatric drugs may disrupt menstruation.
- Chronic systemic diseases: Diabetes, liver or kidney disease can impact menstrual function.
- Eating disorders: Anorexia nervosa or bulimia cause hormonal imbalances that affect the menstrual cycle.
- Pregnancy-related issues: Early pregnancy bleeding, miscarriage, or ectopic pregnancy may present as irregular bleeding.
Risk Factors
- Adolescence and perimenopause: Periods are often irregular during these physiological transition phases.
- Obesity or significant changes in body weight: Both can influence hormonal balance.
- High physical activity levels: Athletes or women with very active lifestyles may have disrupted cycles.
- Chronic medical conditions affecting hormonal or metabolic balance.
- Family history of menstrual disorders or endocrine diseases.
- Psychological stress or psychiatric illnesses.
- Use of certain medications that interfere with hormone function.
Complications
Irregular periods, especially if prolonged or untreated, may lead to:
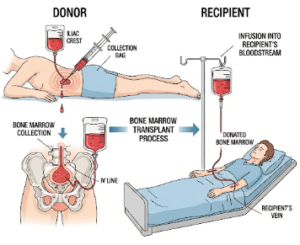
- Anemia: Due to heavy or prolonged menstrual bleeding, causing fatigue and reduced quality of life.
- Fertility issues: Inconsistent ovulation or anovulation reduce chances of conception.
- Endometrial hyperplasia and cancer: Unopposed estrogen stimulation of the uterine lining in anovulatory cycles increases cancer risk.
- Bone density loss: Particularly in cases of amenorrhea related to low estrogen levels, increasing osteoporosis risk.
- Psychological impact: Anxiety, depression, and social distress associated with chronic menstrual problems.
- Cardiometabolic risks: Conditions like PCOS increase risks for diabetes, hypertension, and cardiovascular diseases.
Prevention
- Maintain a healthy lifestyle: Balanced diet, regular exercise, and healthy body weight.
- Manage stress effectively through relaxation techniques and counseling.
- Avoid excessive or sudden weight changes.
- Timely medical consultation for menstrual abnormalities.
- Use hormonal contraception judiciously under medical guidance.
- Regular health check-ups to detect and manage endocrine or systemic disorders early.
- Education on menstrual health and self-monitoring.
Treatment Options in Korea
In Korea, the management of irregular periods is tailored to the underlying cause and patient needs:
- Comprehensive Diagnostic Workup:
- Detailed history taking and physical examination.
- Hormonal assays including FSH, LH, prolactin, thyroid function tests, and androgens.
- Pelvic ultrasonography to evaluate ovaries and uterus for cysts, fibroids, or other pathologies.
- Endometrial sampling when indicated.
- Imaging studies for pituitary tumors if hyperprolactinemia is suspected.
- Medical Management:
- Hormonal therapies:
- Combined oral contraceptives to regulate cycles, reduce bleeding, and treat hormonal imbalances.
- Progesterone or progestin-only therapy for amenorrhea or endometrial protection.
- Metformin for PCOS to improve insulin resistance and restore ovulation.
- Treatment of endocrine disorders: Thyroid hormone replacement or dopamine agonists for prolactinomas.
- Iron supplementation: For anemia secondary to heavy bleeding.
- Lifestyle interventions: Nutritional counseling and weight management support.
- Psychological support: Addressing stress or mood disorders linked to menstrual irregularities.
- Hormonal therapies:
- Surgical Interventions:
- Myomectomy or polypectomy for fibroids and polyps causing abnormal bleeding.
- Endometrial ablation or hysteroscopic procedures in refractory cases.
- Laparoscopic surgery for ovarian cysts or endometriosis.
- Fertility Treatment:
- Ovulation induction with clomiphene citrate or letrozole for women desiring pregnancy.
- Assisted reproductive technologies where appropriate.
- Follow-up and Monitoring:
- Regular follow-up visits to monitor treatment response and modify therapy as needed.
- Screening for complications such as anemia or endometrial pathology.