Overview
Iridodialysis is an ocular condition characterized by the partial or complete detachment of the iris from its root at the ciliary body. This disruption occurs primarily due to trauma but can also arise from surgical complications or penetrating eye injuries. The iris plays a crucial role in regulating the amount of light entering the eye by controlling pupil size. When iridodialysis occurs, this function is compromised, leading to visual disturbances such as irregular pupil shape, light sensitivity, and sometimes decreased vision. If untreated or severe, it can cause secondary complications like glaucoma or cataracts. In Korea, highly skilled ophthalmologists utilize advanced diagnostic imaging and microsurgical techniques to effectively diagnose and treat iridodialysis, improving functional and cosmetic outcomes for patients.
What is Iridodialysis?
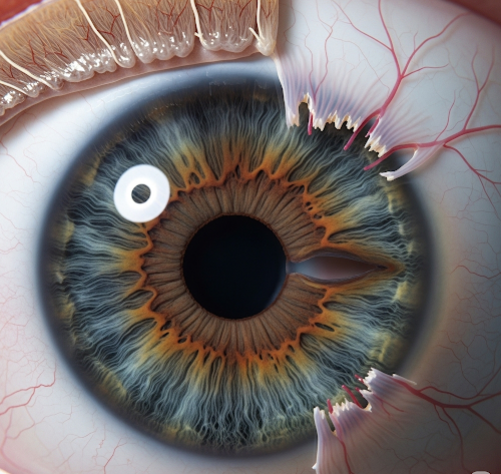
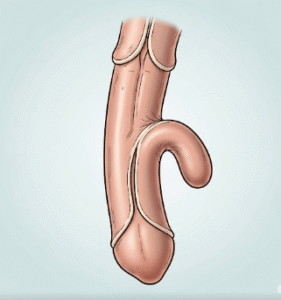
Iridodialysis refers to the tearing or separation of the iris at its root from the ciliary body, the structure that anchors the iris to the eye wall. This injury disrupts the circular integrity of the iris and alters pupil anatomy, resulting in an abnormal pupil shape—often described as a “keyhole” or “D-shaped” pupil. The degree of iridodialysis can vary from a small localized detachment to a complete 360-degree separation.
The condition affects the iris’s ability to constrict and dilate properly, impairing the eye’s natural regulation of light. This can cause light to enter through the gap created by the detached iris, leading to glare, halos, and photophobia. Iridodialysis also alters the eye’s optics and may be associated with other traumatic injuries such as hyphema (blood in the anterior chamber), lens damage, or retinal injury.
Symptoms
The symptoms of iridodialysis depend largely on the extent of the injury and whether other ocular structures are involved:
- Irregular pupil shape: Patients often notice a keyhole or D-shaped pupil on the affected eye, which may be visible cosmetically.
- Photophobia: Increased light sensitivity is common due to abnormal light entry through the gap in the iris.
- Glare and halos: Visual disturbances caused by stray light entering the eye.
- Blurred or reduced vision: May result from the injury itself or secondary complications.
- Monocular diplopia (double vision): Caused by distorted pupil shape and irregular light refraction.
- Eye pain or discomfort: Particularly soon after trauma.
- Redness and swelling: Signs of acute inflammation or hyphema.
- Floaters or flashes: If retinal involvement occurs.
Causes
Iridodialysis most commonly results from:
- Blunt ocular trauma: This is the predominant cause, often due to sports injuries, motor vehicle accidents, physical assault, or accidental impact. The sudden force displaces the iris from its root.
- Penetrating eye injuries: Such as lacerations or foreign body penetration through the cornea or sclera, which physically disrupt iris attachments.
- Intraocular surgeries: Complications during cataract extraction, glaucoma filtering surgeries, or other anterior segment procedures can inadvertently damage the iris root.
- Secondary causes: Rarely, spontaneous iridodialysis may occur in association with severe ocular inflammation or degenerative eye diseases.
Risk Factors
- History of ocular trauma or previous eye surgery.
- Participation in high-risk activities: Contact sports, construction work, or occupations with risk of eye injury.
- Lack of protective eyewear during hazardous tasks.
- Pre-existing ocular conditions: Weak iris root attachments or degenerative changes.
- Systemic conditions: Diabetes or hypertension that may impair healing.
Complications
Iridodialysis can give rise to various complications that affect vision and eye health:
- Persistent irregular pupil: Leading to cosmetic concerns and functional problems such as poor vision in bright light or glare.
- Photophobia: Often severe, affecting daily activities.
- Hyphema: Blood in the anterior chamber can increase intraocular pressure and cause further damage.
- Secondary glaucoma: Angle recession or damage to the trabecular meshwork can lead to increased intraocular pressure and optic nerve damage.
- Cataract formation: Trauma-induced lens opacities may develop over time.
- Retinal detachment or vitreous hemorrhage: If trauma extends to posterior segment.
- Chronic anterior uveitis: Persistent inflammation may cause further ocular damage.
Prevention
Preventing iridodialysis focuses primarily on minimizing eye trauma risk:
- Wearing protective eyewear: Goggles or face shields during sports, industrial work, or hazardous activities.
- Prompt evaluation of any eye injury: Early treatment can prevent complications.
- Safe surgical techniques: Utilizing advanced microsurgical instruments and experienced surgeons reduces iatrogenic injury risk.
- Public awareness: Education about eye safety in high-risk populations.
Treatment Options in Korea
Korean ophthalmology centers provide comprehensive care for iridodialysis with cutting-edge diagnostic tools and surgical expertise:
- Diagnostic Evaluation:
- Slit-lamp biomicroscopy: Essential to visualize iris root detachment, assess pupil shape, and detect concurrent anterior segment injuries.
- Gonioscopy: Evaluates the anterior chamber angle for recession or damage that could cause glaucoma.
- Anterior segment optical coherence tomography (AS-OCT): Provides high-resolution cross-sectional images of the iris, ciliary body, and angle structures, aiding in precise assessment.
- Ultrasound biomicroscopy: Useful for evaluating structures obscured by blood or swelling.
- Fundus examination: To rule out posterior segment trauma.
- Medical Management:
- Symptomatic relief: Artificial tears, sunglasses, and tinted lenses to reduce photophobia and glare.
- Anti-inflammatory agents: Topical corticosteroids for inflammation control when necessary.
- Intraocular pressure control: Medications to manage secondary glaucoma if present.
- Observation: Small, asymptomatic iridodialysis without visual impairment may be monitored.
- Surgical Intervention:
- Iris repair surgery: Recommended for large or visually significant iridodialysis causing functional impairment or cosmetic defects.
- Techniques:
- Iris suturing to reattach the iris root to the scleral spur or ciliary body using fine microsurgical sutures.
- Pupil reconstruction procedures to restore near-normal shape and function.
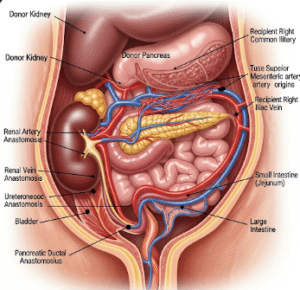
- Adjunctive surgeries: Cataract extraction or glaucoma filtering procedures if secondary complications arise.
- Korea’s ophthalmic surgeons utilize advanced microsurgical microscopes and techniques to maximize functional and aesthetic outcomes while minimizing risks.
- Postoperative Care and Rehabilitation:
- Frequent follow-up to monitor for infection, inflammation, intraocular pressure changes, and visual recovery.
- Visual rehabilitation including corrective lenses or low vision aids if needed.
- Psychological support addressing cosmetic concerns and quality of life.