Overview
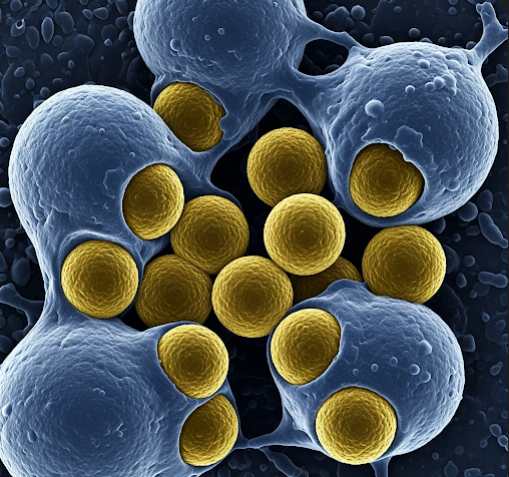
Invasive staphylococcal infections are serious infections caused by Staphylococcus aureus bacteria that penetrate beyond the skin into deeper tissues, the bloodstream, or organs. These infections can lead to severe complications such as sepsis, pneumonia, or bone infections and require prompt medical attention. In Korea, advances in diagnostic techniques and antibiotic therapies, combined with hospital infection control measures, play a vital role in managing invasive staph infections effectively.
What Are Invasive Staph Infections?
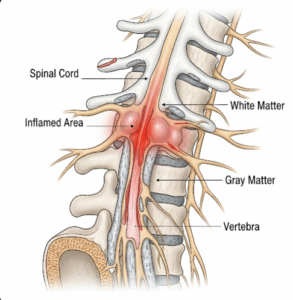
Staphylococcus aureus is a common bacterium found on the skin and mucous membranes of healthy individuals. While usually harmless on the surface, it can become invasive if it enters the body through cuts, wounds, or medical devices. Invasive staph infections occur when the bacteria invade sterile parts of the body such as the bloodstream (bacteremia), bones (osteomyelitis), heart valves (endocarditis), lungs (pneumonia), or surgical sites, causing systemic illness.
Symptoms
Symptoms vary based on the infection site but may include:
- Fever and chills
- Localized pain, redness, swelling, and warmth
- Fatigue and malaise
- Rapid heart rate and low blood pressure in severe cases (sepsis)
- Difficulty breathing in pneumonia
- Joint pain and swelling if septic arthritis develops
- Confusion or altered mental status in severe infections
Causes
The infection typically arises when Staphylococcus aureus enters the body via:
- Skin injuries such as cuts, abrasions, or surgical wounds
- Insertion of medical devices like catheters or prosthetic implants
- Intravenous drug use
- Spread from localized skin infections like abscesses or boils
- Hospital environments, especially in patients with weakened immune systems
Risk Factors
- Hospitalization and invasive procedures
- Presence of indwelling medical devices
- Immunocompromised states including diabetes, cancer, or HIV infection
- Recent surgery or trauma
- Intravenous drug use
- Chronic illnesses such as renal failure or lung disease
- Previous staph colonization or infections
Complications
- Sepsis and septic shock, potentially life-threatening systemic infections
- Endocarditis causing heart valve damage
- Osteomyelitis or septic arthritis leading to bone and joint destruction
- Abscess formation in internal organs
- Respiratory failure due to severe pneumonia
- Recurrence and antibiotic resistance, including MRSA (methicillin-resistant Staphylococcus aureus) strains
Prevention
- Rigorous hand hygiene in healthcare settings
- Proper wound care and timely treatment of skin infections
- Use of sterile techniques during surgeries and device insertions
- Screening and decolonization protocols for high-risk patients
- Judicious use of antibiotics to prevent resistance
- Education on safe injection practices for intravenous drug users
Treatment Options in Korea
Korea’s healthcare system offers comprehensive management of invasive staph infections through:
- Diagnostics:
- Blood cultures, imaging studies, and tissue biopsies to identify infection source and severity
- Antibiotic susceptibility testing to guide targeted therapy
- Antibiotic Therapy:
- Empirical broad-spectrum antibiotics initially, later tailored based on culture results
- Use of agents effective against MRSA, such as vancomycin or linezolid, when indicated
- Prolonged intravenous antibiotic courses depending on infection site
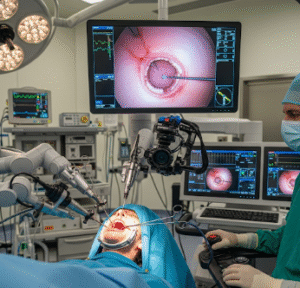
- Surgical Intervention:
- Drainage of abscesses or removal of infected prosthetic devices
- Debridement of infected tissues to control the source
- Supportive Care:
- Management of complications like sepsis in intensive care units
- Monitoring for organ function and addressing systemic effects
- Infection Control:
- Hospital protocols to prevent spread of resistant strains
- Patient education on hygiene and wound care post-discharge
Korean hospitals combine cutting-edge medical treatments with strict infection control policies to reduce the burden of invasive staph infections and improve patient outcomes.