Overview
Invasive lobular carcinoma (ILC) is the second most common subtype of invasive breast cancer, comprising approximately 10-15% of all cases. Unlike invasive ductal carcinoma (IDC), ILC originates in the lobules, the milk-producing glands of the breast, and is known for its distinctive growth pattern. Instead of forming a defined lump, ILC tends to grow in a diffuse, infiltrative “single-file” pattern due to the loss of cell adhesion molecules. This unique behavior often makes early detection more challenging. ILC is often hormone receptor-positive and HER2-negative, which influences treatment decisions. In Korea, enhanced imaging technologies, molecular testing, and multidisciplinary treatment approaches have significantly improved early detection, personalized therapies, and survival rates for patients with ILC.
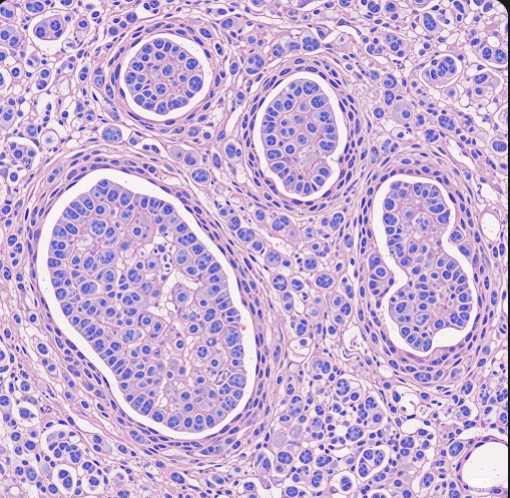
What is Invasive Lobular Carcinoma?
ILC develops from the lobular epithelial cells lining the breast lobules. These cells normally produce milk during lactation. Unlike other breast cancers, ILC is characterized by the loss of E-cadherin, a protein essential for cell-to-cell adhesion. This loss results in discohesive cancer cells that invade breast tissue in thin linear chains, making it less likely to form a palpable mass and more prone to multifocal (multiple tumors in one breast) or multicentric (tumors in different quadrants) disease.
Because of this growth pattern, ILC tumors are often bilateral (present in both breasts) and can be underestimated on routine imaging such as mammography, necessitating the use of breast MRI for more accurate detection.
Symptoms
Symptoms of ILC are often subtle and may be overlooked during early stages:
- Diffuse thickening or fullness of the breast rather than a distinct lump.
- Changes in breast size or shape, including asymmetry between breasts.
- Skin changes, such as mild dimpling or puckering (peau d’orange).
- Nipple changes, such as inversion or mild discharge, though less common compared to other breast cancers.
- Swelling or palpable lumps in the axillary (underarm) lymph nodes, indicating possible lymphatic spread.
- In some cases, ILC may be detected incidentally on imaging before symptoms develop.
Because ILC can grow in a subtle, infiltrative pattern, patients and clinicians may not notice symptoms until the disease has advanced.
Causes
The exact causes of ILC are multifactorial and include genetic, hormonal, and environmental influences. The hallmark molecular event in ILC is the loss or inactivation of the E-cadherin gene (CDH1), which disrupts cell adhesion and facilitates the invasive growth pattern.
Other contributing factors:
- Accumulation of genetic mutations in breast epithelial cells over time.
- Hormonal influences, especially prolonged estrogen exposure.
- Possible interactions between genetic predisposition and lifestyle or environmental factors.
Risk Factors
Risk factors for ILC overlap with those of other breast cancers but have some distinct features:
- Age: ILC is more common in women over 50, particularly postmenopausal.
- Hormonal exposure: Long-term hormone replacement therapy (HRT), especially combined estrogen-progestin therapy, increases risk.
- Family history: Having first-degree relatives with breast cancer raises the risk.
- Genetic mutations: Mutations in BRCA1, BRCA2, and CDH1 genes, the latter specifically associated with lobular carcinoma.
- Reproductive history: Late age at first childbirth or nulliparity (no childbirth).
- Lifestyle factors: Obesity, alcohol consumption, and physical inactivity.
- Breast density: Higher breast density on mammograms may increase risk.
- Previous breast lesions: Lobular carcinoma in situ (LCIS) is a recognized precursor lesion increasing future risk of ILC.
Complications
Without timely diagnosis and treatment, ILC can lead to several serious complications:
- Local tissue invasion: Because ILC often grows diffusely, it can involve large areas of the breast, leading to extensive tissue distortion.
- Lymph node involvement: Spread to axillary lymph nodes occurs frequently and worsens prognosis.
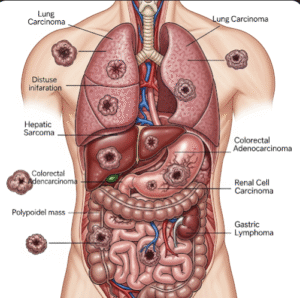
- Distant metastasis: ILC has a predilection for spreading to unusual sites including bones, gastrointestinal tract, peritoneum, ovaries, and leptomeninges, differing from the typical lung and liver metastases of ductal carcinoma.
- Recurrence: ILC tends to recur locally or distantly many years after initial treatment due to its indolent and infiltrative nature.
- Treatment-related effects: Surgical complications, chemotherapy or hormonal therapy side effects, and radiation-induced skin or tissue changes.
Prevention
Although ILC cannot be entirely prevented, several measures can reduce risk and improve early detection:
- Regular breast cancer screening: Mammograms starting at recommended ages, supplemented by breast MRI in high-risk women or when mammography is inconclusive.
- Lifestyle modifications: Maintaining healthy weight, exercising regularly, limiting alcohol intake, and avoiding tobacco use.
- Hormone therapy management: Limiting the duration of hormone replacement therapy and discussing alternatives with healthcare providers.
- Genetic counseling and testing: For women with family history or identified genetic mutations.
- Close monitoring of women with precursor lesions: Such as lobular carcinoma in situ (LCIS).
Treatment Options in Korea
Korea has developed comprehensive breast cancer care systems equipped with advanced diagnostics and personalized treatment plans tailored to ILC’s unique behavior:
- Diagnostics:
- Mammography and breast ultrasound: Initial imaging tools, though often limited in detecting ILC.
- Breast MRI: Offers high sensitivity for identifying multifocal, multicentric, and bilateral lesions, guiding surgical planning.
- Core needle biopsy: Essential for histopathological diagnosis and assessment of hormone receptor (ER, PR) and HER2 status.
- Genetic testing: For selected patients to identify hereditary cancer syndromes.
- Surgical Management:
- Breast-conserving surgery (lumpectomy): Possible for localized disease but may require wide excision due to diffuse growth.
- Mastectomy: Often recommended for multifocal, multicentric, or bilateral disease.
- Sentinel lymph node biopsy and axillary dissection: To evaluate and manage lymph node involvement.
- Reconstructive surgery: Available post-mastectomy for cosmetic and psychological benefits.
- Systemic Therapy:
- Hormonal therapy: Most ILC tumors are estrogen and progesterone receptor positive, responding well to endocrine therapies such as tamoxifen or aromatase inhibitors.
- Chemotherapy: Considered based on tumor size, grade, and nodal status, though ILC tends to be less responsive than ductal carcinoma.
- Targeted therapies: Rarely needed as HER2 positivity is uncommon in ILC.
- Emerging treatments: Research in molecular profiling may guide novel therapies in the future.
- Radiation Therapy:
- Indicated after breast-conserving surgery and in selected post-mastectomy cases to reduce local recurrence.
- Follow-up and Surveillance:
- Lifelong monitoring with regular clinical exams and imaging due to the risk of late recurrence.
- Supportive care addressing side effects and quality of life.
- Multidisciplinary Care Teams:
- Korean breast cancer centers integrate surgeons, medical oncologists, radiation oncologists, radiologists, pathologists, genetic counselors, and supportive care specialists to deliver holistic, patient-centered care.