Overview
Invasive ductal carcinoma (IDC) is the most common type of breast cancer, accounting for about 70-80% of all breast cancer cases worldwide. IDC begins in the milk ducts of the breast but invades surrounding breast tissue, potentially spreading to lymph nodes and other organs if left untreated. Early diagnosis and treatment are critical to improving survival rates. In Korea, advances in breast cancer screening, imaging, pathology, and treatment options have greatly enhanced the management and prognosis of IDC, with multidisciplinary care centers providing personalized treatment plans for patients.
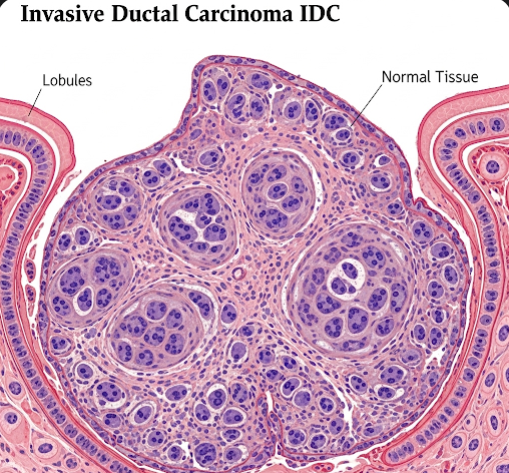
What is Invasive Ductal Carcinoma?
Invasive ductal carcinoma originates from the epithelial cells lining the milk ducts of the breast. Unlike ductal carcinoma in situ (DCIS), where cancer cells are confined within the ducts, IDC breaks through the duct walls and infiltrates the surrounding breast tissue, making it invasive. This invasive nature allows cancer cells to enter lymphatic vessels or blood vessels, potentially metastasizing to lymph nodes, bones, lungs, liver, or brain.
IDC can vary in aggressiveness, hormone receptor status (estrogen receptor [ER], progesterone receptor [PR]), and HER2 (human epidermal growth factor receptor 2) expression, which influence treatment strategies and prognosis.
Symptoms
Early IDC may not cause noticeable symptoms and is often detected during routine mammograms. When symptoms occur, they may include:
- A painless, hard lump or mass in the breast.
- Changes in breast size or shape.
- Skin changes over the breast, such as dimpling, redness, or thickening.
- Nipple abnormalities including inversion, discharge, or scaling.
- Swelling or lumps in the underarm (axillary) lymph nodes.
- Breast pain or tenderness (less common).
Causes
The exact cause of IDC is not fully understood, but it arises from genetic mutations in breast ductal epithelial cells that lead to uncontrolled growth and cancer formation. Factors implicated in the development include:
- Accumulation of genetic mutations over time.
- Hormonal influences, particularly prolonged estrogen exposure.
- Environmental factors and lifestyle influences.
- Family history of breast or related cancers.
- Certain inherited gene mutations (e.g., BRCA1, BRCA2).
Risk Factors
Several factors increase the risk of developing IDC:
- Age: Risk increases with age, especially after 40 years.
- Gender: Female gender is predominant; men can develop IDC but it is rare.
- Family history: First-degree relatives with breast cancer raise risk.
- Genetic mutations: BRCA1, BRCA2, and other gene mutations.
- Hormonal factors: Early menstruation, late menopause, hormone replacement therapy.
- Reproductive history: Nulliparity or late first childbirth.
- Lifestyle factors: Alcohol consumption, obesity, sedentary lifestyle.
- Breast density: High mammographic density increases risk.
- Previous breast conditions: History of atypical hyperplasia or DCIS.
Complications
If left untreated or diagnosed late, IDC can cause:
- Local spread: Invasion of chest wall, skin ulceration.
- Lymph node metastasis: Axillary lymph nodes involvement is common.
- Distant metastasis: Spread to bones, lungs, liver, brain causing systemic symptoms.
- Recurrence: Cancer can return locally or in distant organs after treatment.
- Treatment-related complications: Side effects from surgery, chemotherapy, radiation, or hormonal therapy.
Prevention
While IDC cannot be completely prevented, risk can be reduced through:
- Regular screening: Mammograms and clinical breast exams for early detection.
- Healthy lifestyle: Maintaining ideal weight, regular exercise, limiting alcohol.
- Avoiding hormone overexposure: Careful use of hormone replacement therapy.
- Genetic counseling: For individuals with strong family history or known mutations.
- Breastfeeding: May reduce risk.
- Avoiding smoking: Reduces overall cancer risk.
Treatment Options in Korea
Korea offers state-of-the-art treatment for IDC based on tumor characteristics and patient factors:
- Diagnostic Workup:
- Mammography and breast ultrasound: Initial imaging tools.
- Magnetic resonance imaging (MRI): Used for detailed assessment and high-risk patients.
- Biopsy: Core needle biopsy to confirm diagnosis and analyze tumor markers (ER, PR, HER2).
- Staging: CT scans, bone scans, PET-CT to evaluate metastasis.
- Surgical Treatment:
- Breast-conserving surgery (lumpectomy): Removal of tumor with a margin of healthy tissue.
- Mastectomy: Complete removal of breast in larger or multifocal tumors.
- Sentinel lymph node biopsy and/or axillary lymph node dissection: To assess lymph node involvement.
- Systemic Therapy:
- Chemotherapy: Neoadjuvant (before surgery) or adjuvant (after surgery) to kill cancer cells.
- Hormonal therapy: For ER/PR-positive tumors, using agents like tamoxifen or aromatase inhibitors.
- Targeted therapy: HER2-positive tumors treated with trastuzumab, pertuzumab, and newer agents.
- Immunotherapy: For select cases based on biomarkers.
- Radiation Therapy:
- Typically follows breast-conserving surgery or mastectomy in high-risk cases to reduce recurrence.
- Follow-up Care:
- Regular imaging and clinical exams to monitor for recurrence.
- Supportive care and rehabilitation services.
- Multidisciplinary Approach:
- Korean cancer centers provide coordinated care involving surgeons, medical oncologists, radiation oncologists, pathologists, genetic counselors, and supportive care teams.