Overview
Intussusception is a serious gastrointestinal condition characterized by the telescoping of one segment of the intestine into an adjacent distal segment, causing bowel obstruction and potentially compromising blood flow to the affected bowel. It is the leading cause of intestinal obstruction in infants and toddlers, particularly between 6 months and 3 years of age, although it can occur at any age, including adults. Intussusception can rapidly progress from mild symptoms to life-threatening complications such as bowel ischemia, perforation, peritonitis, and septic shock if not treated promptly.
In Korea, the management of intussusception benefits from highly developed pediatric and surgical care infrastructure, incorporating sophisticated imaging techniques, non-invasive reduction procedures, and minimally invasive surgery. This integrated approach ensures high success rates, reduced morbidity, and better long-term outcomes.
What is Intussusception?
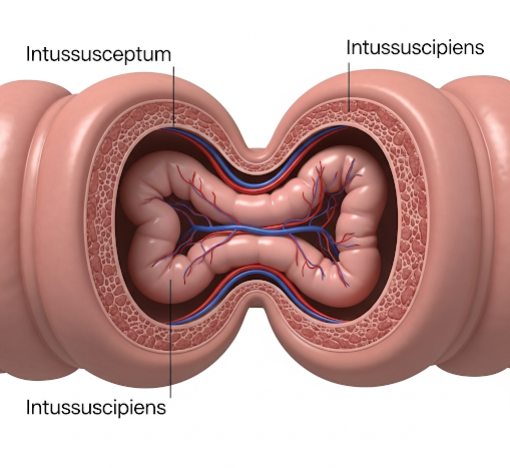
Intussusception involves the invagination or “telescoping” of a proximal portion of the intestine (called the intussusceptum) into the lumen of the immediately adjacent distal portion (intussuscipiens). This creates a segment of bowel folded within itself, leading to obstruction of intestinal contents and venous congestion.
Most commonly, the ileum folds into the colon (ileocolic intussusception), but intussusception can also occur entirely within the small bowel or colon. The invaginated segment pulls the associated mesentery with it, which compromises blood flow, causing swelling, edema, ischemia, and if untreated, necrosis of the bowel wall.
Symptoms
Intussusception symptoms typically develop abruptly and progress rapidly, often following a prodromal illness:
- Paroxysmal abdominal pain: Sudden onset of severe, intermittent, colicky pain causing infants to cry inconsolably, draw up their legs, or double over. These episodes recur every 15-20 minutes.
- Vomiting: Initially non-bilious but often becomes bilious as obstruction progresses.
- “Currant jelly” stool: A late sign characterized by stools mixed with blood and mucus due to bowel ischemia and sloughing of the mucosa.
- Palpable abdominal mass: A sausage-shaped, tender mass is often felt in the right upper or middle abdomen.
- Lethargy or altered consciousness: Especially in infants, possibly due to pain, dehydration, or systemic toxicity.
- Abdominal distension: Develops as bowel obstruction worsens.
- Signs of shock: Including rapid pulse, hypotension, and poor perfusion in advanced disease.
In adults, symptoms may be more chronic or intermittent and often relate to the underlying cause (e.g., tumor).
Causes
The etiology of intussusception varies by age:
- In children: Approximately 90% of cases are idiopathic, with no clear lead point. A common theory implicates hypertrophied Peyer’s patches (lymphoid tissue in the ileum) often enlarged after viral infections (adenovirus, rotavirus), which serve as a lead point causing abnormal peristalsis.
- In adults: Intussusception is rare and usually secondary to a pathological lead point such as benign or malignant tumors, Meckel’s diverticulum, adhesions, or inflammatory lesions.
Other contributing factors:
- Gastrointestinal infections and inflammation.
- Anatomical abnormalities or previous abdominal surgery.
- Cystic fibrosis or other motility disorders.
Risk Factors
- Age: Infants and toddlers aged 6 to 36 months are at highest risk.
- Male gender: Slight male predominance.
- Recent viral illness: Respiratory or gastrointestinal infections.
- Lack of rotavirus vaccination: Some evidence links rotavirus infection to intussusception risk, though the vaccine itself has a very small associated risk.
- Underlying bowel pathology: Especially in adults.
Complications
If intussusception is not promptly diagnosed and treated, several severe complications can occur:
- Bowel ischemia and necrosis: Due to compromised blood supply, leading to tissue death.
- Intestinal perforation: Leakage of intestinal contents causes peritonitis, a life-threatening infection.
- Sepsis and septic shock: Resulting from systemic infection.
- Shock: Due to fluid loss, blood loss, and infection.
- Recurrence: Even after successful treatment, intussusception can recur in up to 10% of cases.
- Long-term bowel dysfunction: Possible if extensive bowel resection is necessary.
Prevention
Preventive measures focus primarily on early detection and management:
- Rotavirus vaccination: Significantly reduces the incidence of rotavirus infections linked to intussusception.
- Prompt treatment of viral gastroenteritis and respiratory infections.
- Careful monitoring: Of infants and young children exhibiting symptoms of abdominal pain, vomiting, or bloody stools.
- Education: Parents should seek early medical attention for sudden, severe abdominal symptoms in children.
Treatment Options in Korea
Korea employs a standardized and effective approach combining early diagnosis, non-surgical management, and surgery when needed:
- Diagnostic Modalities:
- Ultrasound: The gold standard for diagnosis, showing the characteristic “target” or “doughnut” sign. It is non-invasive, radiation-free, and widely available in Korean hospitals.
- Abdominal X-ray: Used to evaluate for obstruction or perforation.
- Contrast or air enema: Both diagnostic and therapeutic, performed under fluoroscopy or ultrasound guidance.
- Non-surgical Reduction:
- Hydrostatic reduction using barium or saline enema.
- Pneumatic (air) enema: Increasingly preferred due to higher success rates and lower complication rates.
- These procedures are performed in radiology suites with continuous imaging to confirm reduction. Success rates exceed 80-90% in uncomplicated cases.
- Patients are closely monitored post-procedure for signs of recurrence or complications.
- Surgical Intervention:
- Indicated if enema reduction fails, signs of perforation or peritonitis develop, or if a pathological lead point is suspected.
- Open laparotomy or laparoscopic surgery is performed to manually reduce the intussusception and resect necrotic or pathological bowel segments.
- Korean surgeons are experienced in minimally invasive techniques, reducing hospital stay and recovery time.
- Post-treatment Care:
- Fluid resuscitation and correction of electrolyte imbalances.
- Antibiotics if bowel necrosis or perforation occurs.
- Nutritional support and monitoring for recurrence.
- Multidisciplinary Team:
- Pediatricians, pediatric surgeons, radiologists, anesthesiologists, and critical care teams collaborate for optimal outcomes.